4173
Validation study of high framerate source localization for MR-guided HDR brachytherapy1Department of Radiotherapy, University Medical Center Utrecht, Utrecht, Netherlands, 2Image Sciences Institute, University Medical Center Utrecht, Utrecht, Netherlands
Synopsis
For the development of MR-guided high-dose-rate (HDR) brachytherapy, the accuracy and precision of an MR-based HDR source localization method were investigated in a phantom study, by a comparison with CT. MR images were acquired for various angulations of the source with respect to B0, and a 3D CT scan was acquired. The MR source positions were compared to the CT source position. The results demonstrated a high, subvoxel accuracy (0.4-0.6 mm) and a high precision (≤0.1 mm) at high temporal resolutions (0.15-1.2 s per slice). This proved that our proposed MR-based source localization method is valuable for MR-guided HDR brachytherapy.
Introduction
In high-dose-rate (HDR) brachytherapy, a radioactive source is temporarily sent into a set of catheters inserted into a tumor, to irradiate the tumor tissue from the inside. MRI is the preferred imaging modality for guidance of the treatment. As part of the development of MR-guided HDR brachytherapy, we have been working on HDR source localization1. HDR source localization can be used for two main goals: I) real-time MR-guided treatment verification by determining the source positions at the moment of irradiation, and II) reconstruction of the source dwell positions after catheter insertion, by localization of a dummy source before the start of irradiation. This second aim is important for treatment planning and could replace a manual catheter reconstruction (concerned with inaccuracies; catheter is often difficult to distinguish), to improve the practical workflow. To be clinically relevant for treatment verification, high temporal and spatial resolutions are required. This study describes a validation (analysis of accuracy and precision) of our proposed MR-based HDR source localization method, by a comparison with CT.Methods
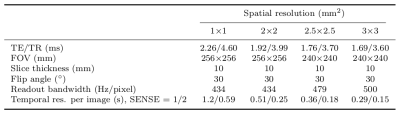
Data acquisition. A non-active iridium brachytherapy source (Elekta NL, Veenendaal, The Netherlands) was positioned in a cylindrical phantom filled with doped water (≈25 mg/l MnCl2), see Fig. 1. The source was placed in the center of a platform, which contains a design of gaps serving as a reference in the images to compare different data sets. MR imaging was performed on a 1.5T MRI system (Ingenia, Philips, Best, The Netherlands), using a 2D dynamic spoiled gradient echo sequence (10 dynamics), see scan parameters in Table 1. Two intersecting slices (coronal/sagittal) were scanned (source cable in-plane), to be able to determine the source position in 3D. For an increased temporal resolution, the spatial resolution was varied and all acquisitions were repeated with parallel imaging (SENSE=2), see Table 1. The influence of these acceleration mechanisms on the localization accuracy was assessed. Furthermore, the influence of variations due to the orientation of the source with respect to the main magnetic field ($$$\overrightarrow{B}_0$$$), affecting the MR artifact, was investigated. The phantom was rotated to vary the angle between the source and $$$\overrightarrow{B}_0$$$ (0°-90°). To validate the localization method, a 3D CT scan was made on a Brilliance Big Bore scanner (Philips, Best, The Netherlands) with voxel size 0.34x0.34x0.40 mm3, using O-MAR for metal artifact reduction. The source position on CT was considered as the gold standard.
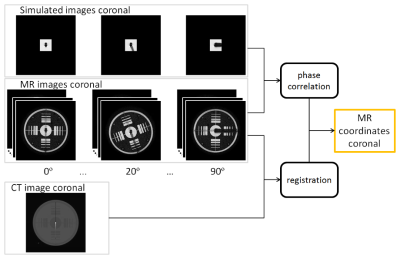
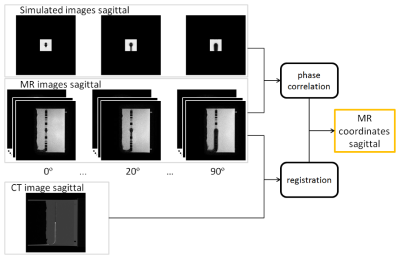
Post processing. Localization of the HDR source was conducted by simulation of the MR artifact (complex data), followed by template matching between the MR images and the simulations using a subpixel phase correlation algorithm to find the translation between the two images1,2,3. This was applied to the coronal and sagittal MR images, see Fig. 2 and Fig. 3. The MR images were registered (translation) to the CT data set (Fig. 2 and Fig. 3). Next, the registered 2D source positions from MRI were combined to the 3D MRI source position.
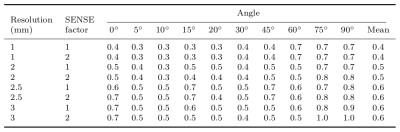
Validation: accuracy and precision. To validate the localization method, the 3D registered MRI source position was compared to the CT source position. The accuracy was calculated as the mean Euclidean distance between the source positions from MRI and CT (over 10 dynamics). The precision was analyzed as the standard deviation over the distances between the positions from MRI and CT (over 10 dynamics).
Results and discussion
The distances between the HDR source positions from MRI and CT are given in Table 2. This showed that the method has a mean accuracy of 0.4-0.6 mm, depending on the resolution, and irrespective of the use of SENSE. The case most plausible for practical application (2 mm resolution and SENSE=2) resulted in a mean accuracy of 0.5 mm at a temporal resolution of 0.25 s per image. Besides, in all cases the standard deviation was ≤0.1 mm, which demonstrates a high precision, meaning that there is almost no variation in repeated measurements.Conclusion
This validation study demonstrated a high, subvoxel accuracy (0.4-0.6 mm) and a high precision (≤0.1 mm) at high temporal resolutions (0.15-1.2 s per slice) for an MR-based HDR source localization method. This means that the method enables an accurate treatment verification and a direct detection of the source dwell positions, important for treatment planning. Hence, MR-based source localization is highly valuable for clinical application in MR-guided HDR brachytherapy. As a first step towards a clinical application, we plan to test the proposed method in a patient study for a direct detection of the source dwell positions (instead of catheter reconstruction), using a dummy source/marker. Acknowledgements
This research was funded by the Eurostars Programme, ITEA3, project name: System of Real-Time Systems (SoRTS), project number: 12026.References
- Beld E. et al. Automatic high temporal and spatial resolution position verification of an HDR brachytherapy source using subpixel localization and SENSE. Proc. Intl. Mag. Reson. Med. 2016; 24: 3585
- Zijlstra F. et al. Fast Fourier-based simulation of off-resonance artifacts in steady-state gradient echo MRI applied to metal object localization. Magn. Reson. Med. 2016; (in press)
- Kuglin C D and Hines D C. The phase correlation image alignment method. Proc. IEEE Int. Conf. Cybernet. Society. 1975; 163-165
Figures