4160
Comparison of MR-guided joint injection with a fluoroscopic approach for pediatric MR arthrography1Radiology, The Children's Hospital of Philadelphia, Philadelphia, PA, United States, 2Siemens Medical Solutions Inc, Hoffman Estates, IL, United States
Synopsis
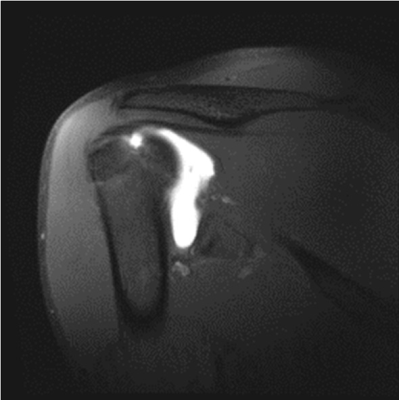
Magnetic resonance imaging (MRI) provides excellent soft-tissue contrast and multiplanar capability in joint imaging, but often requires direct joint injection of gadolinium to provide adequate depiction of cartilage and ligaments. MRI-guided joint interventions are not commonly performed as routine practice. In MR arthrography, the contrast injections are usually performed under fluoroscopy and is followed by a diagnostic MRI to evaluate the abnormalities in the rotator cuffs. This work describes our experience with combined interventional and diagnostic MR shoulder arthrography, and evaluates the efficacy of MR-guided injection, comparing technical success, diagnostic quality, and procedure times to fluoroscopic-guided arthrography.
Introduction/Purpose
MRI guided joint interventions have been reported several years ago but are not routinely performed in daily practice apart from a few centers.1-4 Gadolinium injection for arthrography is conventionally performed under fluoroscopy, with the patient then being transported to MRI.5,6 We report our initial experience with combined MR-interventional and diagnostic shoulder MR arthrography and study the efficacy of MR-guided (MRG) injection, comparing technical success, diagnostic quality, and procedure times to fluoroscopic-guided (FG) injection and subsequent MR arthrography.Methods
MRG injection of the shoulder performed on pediatric patients from Jan-Oct 2017 were included, as were age-matched FG injections from Jan 2016-Feb 2017. Technical success, complications and procedure times were compared. Diagnostic scans were evaluated by a musculoskeletal radiologist, using a Likert score for joint distension (grade 1: optimal; grade 0: sub-optimal), and contrast extravasation (grade 0: none; 1: linear needle tract; 2: fibers <5 cm; 3: fibers >5 cm).Results
39 patients (mean age 16 years; mean weight 72 kg) underwent MRG injection on a 3 Tesla scanner and 42 patients underwent FG injections (mean age 17 years; mean weight 67 kg). Procedure technique was similar between groups, with an anterior approach in all cases. Gadolinium was injected using a 20 G 10 cm MR-compatible needle in MRG cases and a 22 G 3.5 inch BD spinal needle in FG cases.
Technical success rates were 97.4% in MRG and 100% in FG procedures, with one MRG procedure aborted due to sedation reaction. There were no immediate procedure-related complications for either modality. FG cases had mean radiation dose of 5.42 µGym2 (0.1-86 µGym2). The mean interventional procedure time for FG arthrograms was significantly lower than for MRG (16±10 min vs. 23±13 min, p=0.01), but the total interventional and diagnostic MRI procedure time was significantly lower for MRG cases compared to FG cases (57±14 min vs. 78±21 min, p<0.05). Mean transition time from the procedure to diagnostic MR scan was significantly lower in MRG cases compared to FG cases (8±6 min vs. 31±17 min, p<0.05).
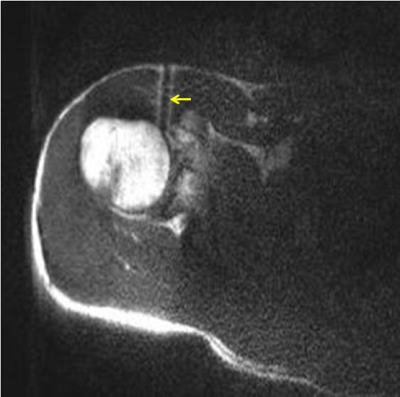
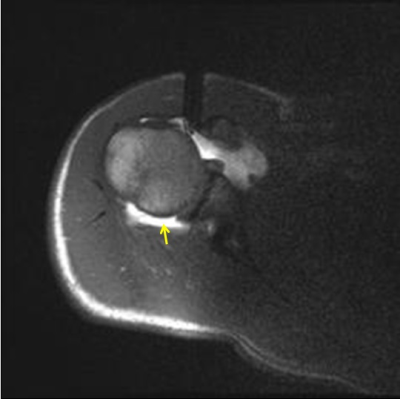
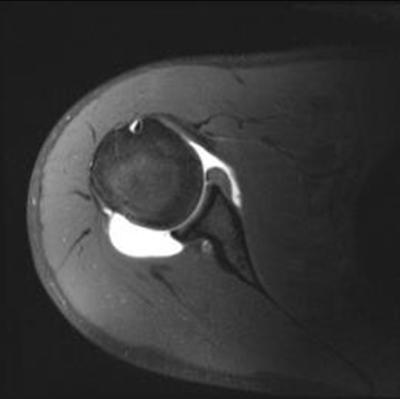
In all MRG and FG cases, the joint distension was optimal. Gadolinium extravasation rates were also similar between the groups: grade 0 in one FG case (2%); grade 1 in 24 MRG (63%) and 28 FG cases (67%); grade 2 in 9 MRG (24%) and 10 FG cases (24%), grade 3 in 5 MRG (13%) and 3 FG cases (7%). The diagnoses were: Normal: 4 (MRG), 7 (FG); labral tear: 23 (MRG) and 20 (FG); and other lesions (shoulder impingement/ dislocation, torn ligament, etc.): 11 (MRG) and 15 (FG). On follow-up, one patient who underwent MRG arthrogram reported new pain attributable to the procedure.
Discussion/Conclusion
MRG injection of the shoulder can be successfully performed with low complications, real-time visualization of the needle and contrast, no ionizing radiation exposure and potential increased workflow efficiency. Technical success and diagnostic adequacy was similar among both modalities. The total interventional and diagnostic MRI procedure time for MRG procedures was significantly lower than the FG procedures. Performance of the interventional procedure and diagnostic scan in the same suite may increase patient throughput. Procedure times suggest MR-guided joint injections may be a feasible entry procedure in instituting an interventional MRI service.Acknowledgements
No acknowledgement found.References
1. T. Schulz, R.B. Trobs, J.P. Schneider, W. Hirsch, S. Puccini, F. Schmidt, T. Kahn. Pediatric MR-guided interventions. Eur J Radiol. 2005; 53(1):57-66.
2. Kevin A. Smith, MD and John Carrino, MD. MRI-Guided Interventions of the Musculoskeletal System. J Magn Reson Imaging. 2008; 27(2):339-46.
3. Garmer M, Grönemeyer D. Magnetic resonance-guided interventions of large and small joints. Top Magn Reson Imaging. 2011; 22(4):153-69.
4. Fritz J, U-Thainual P, Ungi T, Flammang AJ, Fichtinger G, Iordachita II, Carrino JA. Augmented reality visualization with use of image overlay technology for MR imaging guided interventions: assessment of performance in cadaveric shoulder and hip arthrography at 1.5 T. Radiology. 2012; 265(1):254-9.
5. Theodore B. Gupton Jr., Jorge Delgado, Diego Jaramillo, Anne M. Cahill, Nancy A. Chauvin. Comparative analysis of anterior and posterior contrast injection approaches for shoulder MR arthrograms in adolescents. Pediatr Radiol. 2016; 46(13):1848-1855.
6. Perdikakis E, Drakonaki E, Maris T et al. MR arthrography of the shoulder: tolerance evaluation of four different injection techniques. Skelet Radiol. 2013; 42:99–105.
Figures