4155
Percutaneous MR-guided Interventions Using an Optical Moiré Phase Tracking System1Biomedical Magnetic Resonance, Otto-von-Guericke University, Magdeburg, Germany, 2Department of Radiology, Hannover Medical School, Hannover, Germany
Synopsis
The development of an appropriate guidance support is essential to simplify and shorten MRI guided percutaneous interventions. We present a new tracking system and sequence enabling intuitive, interactive and precise instrument navigation with the aid of an optical Moiré Phase tracking system from the inside of the MRI scanner. The system was evaluated regarding targeting error and skin to target time by experienced interventional radiologist and novice users, revealing a precise (0.99mm±0.47mm), fast (155s±62s) and simple real-time needle guidance.
Purpose
MRI as guidance tool for minimally invasive procedures is characterized by
an excellent soft-tissue contrast and lack of ionizing radiation. However,
interventional MRI (iMRI) using the freehand technique is still limited to
specialized clinical centers due to access and workflow limitations1-3. In
particular, manual slice adjustment during the freehand procedure can quickly
become cumbersome and time-consuming without an experienced and well-coordinated
team – even more for complex needle trajectories4.The development of an
appropriate guidance support is essential to simplify and shorten the
intervention. We describe the development and evaluation of a method enabling
intuitive instrument and imaging navigation with the aid of an optical Moiré
Phase Tracking (MPT) system.Methods
For
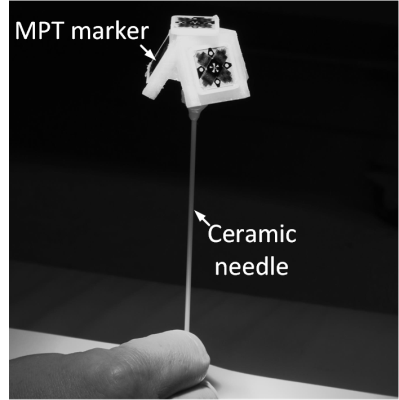
real time needle guidance four MPT markers were rigidly attached to a ceramic
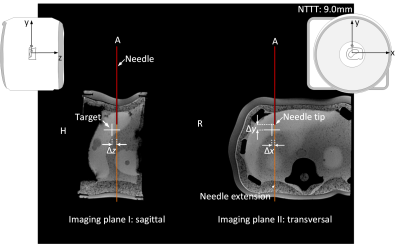
needle (see Fig. 1). A gradient echo sequence was modified to align two
perpendicular imaging planes along the calibrated ceramic needle centered at
the needle tip. The imaging planes are updated according to the pose of the MPT
markers being tracked by a newly developed camera system. For user guidance,
additional information about the needle (red line), its extension (orange line)
and the position of a predefined target (white cross) were added as image
overlay (see Fig. 2). The color of the target cross was changed from white (d>5mm) over orange (3mm<d≤5mm) to yellow (1mm<d≤3mm) and finally to green (≤1mm) depending on the needle tip to target distance d. The tracking information was further
utilized to change the color of the needle extension, indication trajectory
deviations from the planned needle path. The remaining puncture track distance Δy
from the needle tip to the target was added as text overlay ‘NTTT: 9.0mm’ (see
Fig. 2). Both, images and guiding information were displayed on the in-room
monitor to facilitate MRI guided interventions. The sequence (TA=1s,
TE/TR=3.78ms/8ms, 2.08mmx2.08mmx5mm) was evaluated by four experienced
interventional radiologists (experts) and four novices puncturing rubber O-ring
within in a custom-made phantom on a 3T wide-bore MRI systems (80 punctures).
The mean skin to target time was recorded for each user. The user error, system
error and total error were estimated based on a high-resolution 3D validation
dataset.Results
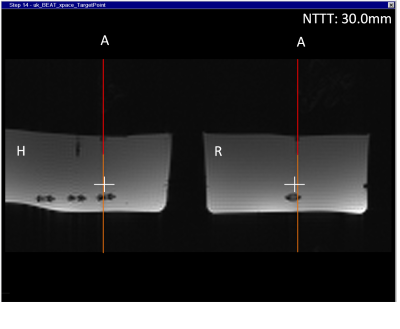
Based
on the constant feedback about the needle, its extension and the target tip
distance, the users easily corrected deviation from the intended trajectory on
the fly (see Fig. 3). The mean skin to target time was 146s±68s for the experts
and 165s±55s for the novices. The mean user error, indicating how well the user
exploited the graphical overlay of the real-time needle guidance, amounted to 0.93mm±0.46mm
for novices being slightly lower for the experts (0.90mm±0.39mm). The system
error, describing the accuracy of the cross-calibration between the MRI and the
optical tracking system as well as the needle calibration, was correspondingly
low for both, experts (0.55mm±0.27mm) and novices (0.50mm±0.27mm). There was
hardly any difference noticeable regarding the total error between the true needle
tip and the predefined target between novices (1.00mm±0.51mm) and experts (0.99mm±0.45mm).Discussion
The
proposed guidance support is proven to be so simple and intuitive that even
novices can achieve similar results as experts in terms of speed and accuracy. The
mean total error presented in other publications4-7 ranged from 1.1mm to
3.9mm. The presented system offers higher accuracy and exact instrument
positioning with a mean total error of 0.99mm±0.47mm for all users. The mean
skin to target time for all users (155s±62s) was slightly higher when compared
to Rothgang et al. (100s± 50s), which
may be explained by the lower acquisition frame rate of the GRE sequence (1fps
vs. 2fps)4. Still, the combination of high accuracy and acceptable skin to
target time, even with the current system, makes the MPT system an attractive
tool not only for experts but also for less-trained interventional
radiologists, who benefit from the intuitive guidance interface. In addition,
the interventional radiologist is able to interactively control the slice plane
position by the interventional instrument itself inside the magnet simplifying
the interaction.Conclusion
In conclusion we developed and evaluated an intuitive, interactive and precise real-time guidance support using the optical MPT system. The proposed approach has the potential to facilitate iMRI-based percutaneous interventions in the future.Acknowledgements
This work was funded by the Federal Ministry of Education and Research within the Forschungscampus STIMULATE under grant number '13GW0095A' and '13GW0095C’.References
1. Hushek SG, Martin AJ, Steckner M, Bosak E, Debbins J, Kucharzyk W. MR systems for MRI-guided interventions. J Magn Reson Imaging 2008; 27:253–266.
2. Meyer BC, Brost A, Kraitchman DL, et al. Percutaneous Punctures with MR Imaging Guidance: Comparison between MR Imaging–enhanced Fluoroscopic Guidance and Real-time MR Imaging Guidance. Radiology 2013; 266:912–919.
3. Barkhausen J, Kahn T, Krombach GA, et al. White Paper: Interventional MRI: Current Status and Potential for Development Considering Economic Perspectives, Part 1: General Application. Rofo 2017; 189:611-623.
4. Rothgang E, Gilson WD, Wacker F, et al. Rapid freehand MR-guided percutaneous needle interventions: An image-based approach to improve workflow and feasibility. J Magn Reson Imaging 2013; 37:1202–1012.
5. Wacker FK, Vogt S, Khamene A, et al. An augmented reality system for MR image-guided needle biopsy: Initial results in a swine model. Radiology 2006; 238:497-504.
6. de Oliveira A, Rauschenberg J, Beyersdorff, et al. Automatic passive tracking of an endorectal prostate biopsy device using phase-only cross-correlation. Magn Reson Med 2008; 59:1043-50.
7. Busse
H, Garnov N, Thörmer G, et al. Flexible add-on solution for MR image-guided
interventions in a closed-bore scanner environment. Magn Reson Med 2010; 64:922-928.
Figures