4078
Design And Evaluation Of Head And Neck Low SAR MRI Protocols For Patients With Implanted Electronic DevicesJessica A. Martinez1,2, Kévin Moulin1, Pablo Villablanca1, and Daniel B. Ennis1,2
1Radiological Sciences, UCLA, Los Angeles, CA, United States, 2Bioengineering, UCLA, Los Angeles, CA, United States
Synopsis
Patients with MRI conditional implantable electronic devices (IEDs) will be referred for MRI examinations. Imaging these patients, however, remains a challenge, in part, because there is no framework to follow for designing protocols that meet SAR labeling requirements. The purpose of this work was to generate and test a workflow that can be followed for optimizing protocols to meet a SAR labeling target. Following the workflow, we optimized head and neck protocols to meet whole-body SAR ≤0.1W/kg and head SAR≤0.3W/kg. Each low SAR MRI series was within the conditional SAR labeling while maintaining image quality.
Introduction
Imaging patients with implantable electronic devices (IEDs) such as pacemakers and deep brain stimulators while meeting SAR guidelines is a challenging task. Frequently, FDA labeled “MRI conditional” IEDs are only approved for 1.5T exams under conditions that typically include whole-body (WB-SAR) or head-only SAR (HO-SAR) limits. SAR restrictions depend on the device labeling and some devices have WB-SAR limit as low as 0.1 W/kg and HO-SAR limits ≤0.3 W/kg. Meeting this SAR restriction can be challenging for clinical MRI protocols and device labeling instructions do not provide protocol guidance. In clinical practice, the majority of MRI protocols are optimized for scan efficiency, tissue contrast, and high spatial resolution, but SAR is not typically considered in the absence of an IED so long as conventional FDA SAR limits are met. Furthermore, there are no generalized framework to create MRI protocols for patients with IEDs and ad hoc protocol modifications are needed while scanning to meet the target SAR limit. This can result in a time-consuming scan and potentially compromised image quality. Head and neck MRI exams are the most common referrals for patients with IEDs [1]. Therefore, our objectives were to: 1) Create a process for modify a standard MRI protocol to meet SAR limits; 2) Optimize the manufacturer’s standard head and neck protocols to meet WB-SAR of ≤0.1 W/kg and HO-SAR ≤0.3 W/kg; 3) Compare the image quality of the low SAR protocols to the standard protocols.Methods
MRI protocol optimization followed the workflow shown in Figure 1-A. The governing criteria were: 1) to limit image contrast changes; 2) to reduce spatial resolution <2x; and 3) to limit scan time increases to <2x. Following these guidelines and Figure 1-A, low SAR head and neck protocols were designed with WB-SAR of ≤0.1 W/kg and HO-SAR ≤0.3 W/kg limits. The analyzed sequences are shown in Figure 1-B. Head and neck images for the standard and low SAR protocols were acquired at 1.5T (Avanto Fit, Siemens) using a TX/RX head coil. SAR and B1+RMS were evaluated for each MRI series in healthy volunteers (N=10: 5 head, 5 neck; 176.3±9.5cm/76.3±21.8kg) after obtaining informed consent under an IRB approved protocol. Image quality was scored by an expert radiologist (blinded) on a 5-point Likert scale (5- excellent; 1- poor).Results
An example of parameter modification following Figure 1-A for a head and a neck sequences is shown in Table 1. For the head protocol, all sequences required parameter modification to meet the WB-SAR and HO-SAR targets, except the localizer. After following the workflow, the low SAR T1 SE sagittal sequence could not meet the HO-SAR≤ 0.3 W/kg target and needed to be replaced with a GRE sequence. For the neck protocol, all sequences required parameter modification to meet the WB-SAR and HO-SAR targets, except for the T2 multi-echo 2D (ME2D) axial and the localizer. The scanner reported WB-SAR, HO-SAR, and B1+RMS for the standard and low SAR protocols are shown in Figure 2. For the head study, the applied energy for the standard and low SAR protocols averaged 0.21±0.17 and 0.03±0.01 W/kg for WB-SAR (Figure 2-A); 1.1±.87 and 0.19±0.06 W/kg for HO-SAR (Figure 2-B); and 2.27±1.09 and 0.98±0.15 µT for B1+RMS (Figure 2-C). For the neck study, the applied energy for the standard protocol and low SAR protocols averaged 0.45±0.3 and 0.09±0.01 W/kg for WB-SAR (Figure 2-D); 0.98±0.66 and 0.21±.003 W/kg for HO-SAR (Figure 2-E); and 2.53±1.31 /1.32±0.0.08 µT for B1+RMS (Figure 2-F). Image quality scores are shown in Figure 3. For the head study (Figure 3-A), qualitative scores were the highest for the standard protocol (4.5±0.55) and lower for the LS protocol (4.17±0.41). For the neck study (Figure 3-B), qualitative scores were the highest for the standard protocol (4.57±0.53) and lower for the LS protocol (4.17±0.75). Image quality scores were not significantly different. Example images are shown in Figure 4.Discussion
A workflow for creating low SAR protocols was created and head and neck low SAR protocols were successfully developed for application in patients with IEDs. Each low SAR MRI series was within the conditional labeling of WB-SAR ≤0.1W/kg and HO-SAR ≤0.3 W/kg while maintaining image quality.Acknowledgements
NIH/NHLBI R21 HL127433.References
[1]: Dewey et al, Elsevier.2007; 63:124-7Figures
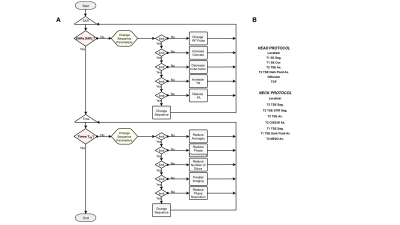
(A) Suggested workflow for SAR optimization while limiting contrast changes, spatial resolution and temporal resolution. (B) Standard head and neck protocols optimized to meet WB-SAR≤0.1 W/kg and HO-SAR≤0.3 W/kg.
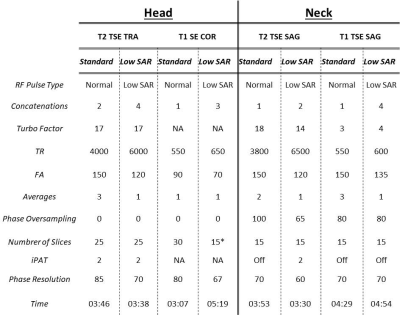
Example of parameter change for achieving WB-SAR≤0.1 W/kg and 0.8 W/kg. * Two parts have been played.
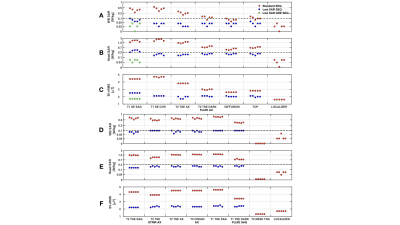
. Scanner reported WB-SAR for (A) head and (D) neck protocols. Scanner
reported HO-SAR for (B) head and (E) neck. Scanner reported B1+RMS for (D) head
and (F) neck. Only the T1 SE sagittal had to be replaced by a GRE sequence. The
dashed line indicates the SAR target.
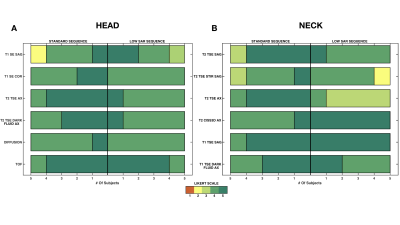
Image quality scoring for the standard and low
SAR sequences for (A) head and (B) neck protocols. Image quality was scored by
an expert for the acquired images on a 5-point Likert scale – 1: Extremely poor (not clinically useful); 2:
Poor (clinical use not recommended); 3: Average (borderline clinical use); 4:
Good; 5: Excellent.
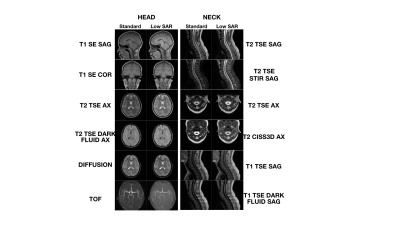
Example images acquired for the standard and low SAR
sequences for head and neck protocols.