3982
Baseline GABA Concentration Predicts Treatment Response to Selective Serotonin Reuptake Inhibitors in Major Depressive Disorder1Radiology, Stony Brook University Hospital, Stony Brook, NY, United States, 2Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 3Psychiatry, Stony Brook University Hospital, Stony Brook, NY, United States
Synopsis
Major depressive disorder (MDD) affects more than 350 million people world-wide. Large heterogeneities in patient symptoms has led to several different treatment courses. Although treatments, such as SSRIs, are generally effective, a large portion of patients (~30%) do not achieve remission. The ability to predict which treatment option will yield the best outcome would be of great use to clinicians and patients. The GABAergic system is implicated in MDD and affected by SSRIs. In this study GABA concentrations were measured with MEGA-PRESS MRS in MDD patients before and after treatment with a SSRI to determine predictive ability and treatment changes.
Introduction:
Major depressive disorder (MDD) is one of the most prevalent and debilitating mental disorders in the world, affecting more than 16 million and 350 million people in the US and world-wide respectively1. The type and severity of symptoms varies between subjects resulting in heterogeneous courses of treatment and outcomes. Although treatments are generally effective, still a large portion of patients (~30%) do not achieve remission. Abnormal GABAergic neurotransmission has been implicated in MDD with several treatments, such as selective serotonin reuptake inhibitors (SSRIs), shown to affect the GABAergic system2. In this study, the predictive power of baseline GABA concentrations to the SSRI treatment response in MDD patients was investigated utilizing MEGA-PRESS MRS.Methods:
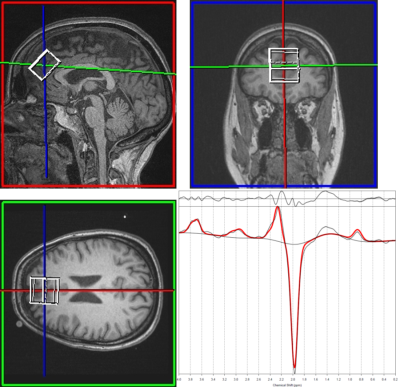
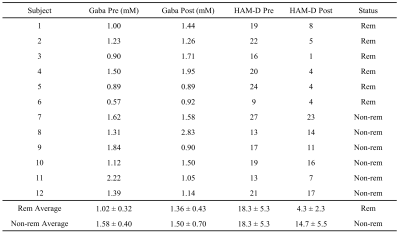
Twelve MDD patients (8 females) were recruited for this IRB-approved study. Patients were imaged at baseline and 8 weeks after treatment with a SSRI (Escitalopram). All patients were assessed with the Hamilton rating scale for depression (HAM-D)3. GABA quantification was performed on Siemens 3T Biograph mMR with a 12-channel head coil. High-resolution T1w MPRAGE images were acquired to localize the MRS voxel to the medial pre-frontal cortex. MEGA-PRESS MRS data were acquired with the following parameters: voxel size of 20×30×20 mm3; TR/TE/ of 1000 ms; 192 repetitions with total acquisition time of ~16 minutes. For absolute quantification of GABA, water-unsuppressed data were also acquired. MEGA-PRESS spectra were processing with a modified GANNET toolbox4 for frequency and phase correction, time averaging and generating difference spectra. The processed difference spectra were fit with TARQUIN5 to quantify GABA concentration. A two-tailed unpaired t-test was performed to test for differences in the mean GABA concentration between responders and non-responders. A two-tailed paired t-test was performed to test for differences in the mean GABA concentration between baseline and post-treatment. P values of <0.05 were considered significant.Results:
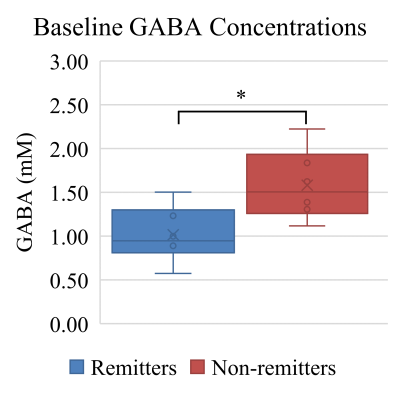
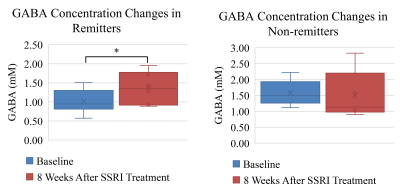
Figure 1 displays MRS voxel placement and the typical MEGA-PRESS difference spectrum from a representative subject. Table 1 lists HAM-D scores and the estimated GABA concentrations at baseline and 8 weeks post-treatment for all 12 patients. 6 patients achieved remission after SSRI treatment; defined as at least 50% decrease in HAM-D score with a post-treatment HAM-D score of at most 10. There is non-significant difference in baseline HAM-D score for remitters and non-remitters (18.3 vs 18.3 p=1). Box plots of baseline GABA concentrations for remitters and non-remitters is shown in Fig 2. Remitters exhibited statistically significant lower baseline GABA concentrations than non-remitters (1.02 vs 1.58 mM, p=0.02). Figure 3 shows box plots of GABA concentrations at baseline and 8 weeks post-treatment for remitters and non-remitters. Patients who achieved remission exhibited a statistically significant increase in GABA concentrations after SSRI treatment (1.02 vs 1.36 mM, p=0.04). A non-significant decrease of GABA concentrations in non-remitters after SSRI treatment was also observed (1.58 vs 1.50 mM, p=0.73).Discussion:
This study investigated GABA concentrations at baseline and 8-weeks post-treatment with a SSRI in patients with MDD. The significant difference in baseline GABA concentrations between remitters and non-remitters suggests that the baseline GABA level can predict the SSRI treatment outcome. These results suggest that lower concentrations of GABA are associated with a more hospitable environment for SSRI’s resulting in greater treatment efficacy. In agreement with other studies in the literature, increased GABA concentrations were observed in remitters after 8 weeks of treatment with a SSRI6. The increase in available serotonin as a result of the SSRI treatment is believed to mediate the excitation of GABAergic interneurons leading to increased GABA concentrations.Conclusion:
Lower baseline GABA concentrations were observed in MDD patients who achieved remission after 8-weeks of treatment with a SSRI. Baseline GABA concentrations have the potential to predict SSRI treatment outcomes for MDD patients.Acknowledgements
No acknowledgement found.References
1. Otte C, Gold SM, Penninx BW, et al. Major depressive disorder. Nature Reviews Disease Primers. 2016;2:nrdp201665.
2. Luscher B, Shen Q, Sahir N. The GABAergic deficit hypothesis of major depressive disorder. Nature Publishing Group; 2011.
3. Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Clinical Psychology. 1967;6(4):278-296.
4. Edden RAE, Puts NAJ, Harris AD, Barker PB, Evans CJ. Gannet: A batch-processing tool for the quantitative analysis of gamma-aminobutyric acid–edited MR spectroscopy spectra. Journal of Magnetic Resonance Imaging. 2014;40(6):1445-1452.
5. Wilson M, Reynolds G, Kauppinen RA, Arvanitis TN, Peet AC. A constrained least-squares approach to the automated quantitation of in vivo 1H magnetic resonance spectroscopy data. Magnetic Resonance in Medicine. 2011;65(1):1-12.
6. Sanacora G, Mason GF, Rothman DL, Krystal JH. Increased occipital cortex GABA concentrations in depressed patients after therapy with selective serotonin reuptake inhibitors. American Journal of Psychiatry. 2002;159(4):663-665.
Figures