3826
Standard Diffusion-Weighted, Diffusion Kurtosis and Intravoxel Incoherent Motion MR Imaging of Sinonasal Malignancies: Correlations with Ki-67 Proliferation Status1Radiology, Eye & ENT Hospital of Fudan University, Shanghai, China, 2Jinshan Hospital of Fudan University, Shanghai, China, 3Siemens Healthcare Ltd., Shanghai, China
Synopsis
This study aimed to explore the correlations between parameters derived from standard diffusion-weighted imaging (DWI), diffusion kurtosis imaging (DKI) and intravoxel incoherent motion (IVIM) with the Ki-67 proliferation status. Our preliminary study shows that DWI-derived parameters from different models are capable of providing different pathophysiological information. DWI, DKI and IVIM parameters are associated with Ki-67 proliferation status. Kmax derived from DKI is the strongest independent factor for the prediction of Ki-67 proliferation status.
INTRODUCTION
The Ki-67 labelling index (LI) has been widely used as a prognostic predictor for many malignant tumours [1-2]. Previous studies have demonstrated that ADC value might be a potential indicator for predicting the Ki-67 LI in various tumours [3]. Several advanced MR techniques with extended diffusion models, including DKI and IVIM, have been proposed to provide a more accurate description of the diffusion behaviour of water molecules within tumours [4-5]. Thus, the purpose of this study is to explore whether quantitative parameters derived from standard DWI, DKI and IVIM can be used to preoperatively suggest the Ki-67 statuses of these patients.MATERIALS AND METHODS
Study population
Eighty-three consecutive patients (between May 2015 and April 2017) with sinonasal solid masses were recruited based on the following inclusion criteria: 1) malignant tumours were histopathologically proven by surgery/biopsy; 2) standard DWI, DKI and IVIM were performed; and 3) an immunohistochemical marker of Ki-67 was available from pathology. The exclusion criteria were as follows: 1) image quality was insufficient due to severe artefacts (n = 3); 2) the lesion was too small (< 10 mm in short-axis diameters) (n = 3); and 3) the patient had a history of treatment or recurrence before MR examinations (n = 2). Ultimately, 75 patients (51 men and 24 women; mean age 52.33 ± 17.74 years; range, 23-82 years) with sinonasal malignant tumours, including squamous cell carcinomas (n = 23), olfactory neuroblastomas (n = 13), malignant melanomas (n = 12), rhabdomyosarcomas (n = 9), malignant lymphomas (n = 6), adenoid cystic carcinomas (n = 5), undifferentiated carcinomas (n = 2), osteosarcomas (n = 2), neuroendocrine carcinomas (n = 2) and malignant fibrohistiocytoma (n = 1), were enrolled in our retrospective study.
MR Techniques
MRI examinations were performed on a 3 T MR scanner (MAGNETOM Verio, Siemens Healthineers, Erlangen, Germany) using a 12-channel head matrix coil. A single-shot echo planar imaging sequence with a pair of rectangular diffusion gradient pulses along all three orthogonal axes was used to obtain isotropic DWI images. The imaging parameters were as follows: TR/TE = 5200/83 ms, number of averages = 2, acquisition matrix = 320 × 256; field of view = 220 mm2, slice thickness = 5 mm, intersection gap = 5 mm, parallel imaging acceleration factor = 2. In addition, 14 different b factors ranging from 0 to 2500 sec/mm2 were used (b = 0, 50, 100, 150, 200, 250, 300, 350, 400, 800, 1000, 1500, 2000, and 2500 sec/mm2).
Image Processing and Analysis
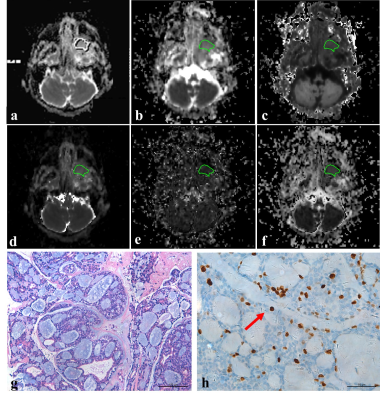
DW images obtained by b = 0 and 1000 sec/mm2 were employed to calculate ADC on an off-line workstation (Verio; Siemens, Erlangen, Germany). Using the signal intensities of six b-values (b = 0, 400, 800, 1000, 2000 and 2500 sec/mm2), DKI parameters were calculated [4]. IVIM parameters can be derived by fitting MR signal acquired at eleven b-values (b = 0, 50, 100, 150, 200, 250, 300, 350, 400, 800 and 1000 sec/mm2) to a bi-exponential model [5]. IVIM and DKI processing was conducted by using MATLAB (version 7.9, MathWorks, Inc., Natick, MA). Five small round ROIs were placed inside the tumours on the corresponding parameter maps. The mean, minimum, and maximum values calculated from DWI (ADC), DKI (Dk, K) and IVIM (D, D* and f) methods were then selected for the analysis. Moreover, one polygonal ROI was also drawn along the outer margin of the lesion on the largest slice of the corresponding parameter maps to calculate the standard DWI, DKI and IVIM parameters for the whole lesion. The Ki-67 LI was categorized as high (> 50%) or low (≤ 50%).
Statistical analyses were performed using simple linear regression analyses, Student’s t-tests and receiver operating characteristic curves analyses.
RESULTS
The K and f values were positively correlated with the Ki-67 LI (r range: 0.288 ~ 0.487), whereas the ADC, Dk and D values were negatively correlated with the Ki-67 LI (r range: -0.403 ~ -0.262). As shown in Figs. 1-2, the ADC, Dk and D values were lower, whereas the K value was higher in sinonasal malignancies with a high Ki-67 LI than those in a low Ki-67 LI (all p < 0.05). A higher maximum K value (Kmax > 0.977) independently predicted a high Ki-67 status (odds ratio [OR] = 7.614; 95% confidence interval [CI] = 2.197-38.674; p = 0.017).DISCUSSION AND CONCLUSIONS
Quantitative MR parameters, such as ADC derived from standard DWI, Dk and K derived from DKI, together with D and f derived from IVIM, were significantly associated with Ki-67 proliferation status in patients with sinonasal malignancies. In particular, a high Kmax value was the strongest independent indicator of a high Ki-67 proliferation status.Acknowledgements
None.References
1. Valente G, Mamo C, Bena A et al (2006) Prognostic significance of microvessel density and vascular endothelial growth factor expression in sinonasal carcinomas. Hum Pathol 37:391-400 2. Airoldi M, Garzaro M, Valente G et al (2009) Clinical and biological prognostic factors in 179 cases with sinonasal carcinoma treated in the Italian Piedmont region. Oncology 76:262-269 3. Driessen JP, Caldas-Magalhaes J, Janssen LM et al (2014) Diffusion-weighted MR imaging in laryngeal and hypopharyngeal carcinoma: association between apparent diffusion coefficient and histologic findings. Radiology 272:456-463 4. Jensen JH, Helpern JA, Ramani A, Lu H, Kaczynski K (2005) Diffusional kurtosis imaging: the quantification of non-gaussian water diffusion by means of magnetic resonance imaging. Magn Reson Med 53:1432-1440 5. Le Bihan D (1988) Intravoxel incoherent motion imaging using steady-state free precession. Magn Reson Med 7:346-351Figures