3818
Intravoxel incoherent motion (IVIM) provides reliable measures of blood volume in patients with metastases to the brain1Diagnostic Physics, Oslo University Hospital, Oslo, Norway, 2Radiology and Nuclear Medicine, Oslo University Hospital, Oslo, Norway, 3Diagnostic Physic, Oslo University Hospital, Oslo, Norway, 4Oslo University Hospital, Oslo, Norway, 5Hospital of Southern Norway, Kristiansand, Norway, 6The Hospital Østfold Kalnes, Kalnes, Norway
Synopsis
In this study, we aimed to assess the potential of using intravoxel incoherent motion (IVIM) for measuring cerebral blood volume (CBV) in brain metastases and normal brain tissue. DWI was acquired with b=0, 200, 300 and 1000s/mm2 in nineteen patients with 23 brain metastases from lung cancer. Asymptotic IVIM fitting yielded an estimation of the perfusion fraction, and subsequent estimation of CBV. CBVDWI in brain metastases and gray matter correlated significantly with CBV obtained from conventional DSC MRI. Our results suggest that IVIM may serve as an independent and reliable surrogate marker of blood volume in well perfused brain tissue.
INTRODUCTION
Diffusion-weighted Imaging (DWI) is a fast and easily accessible technique that has become an essential part of oncological imaging protocols. An increasing number of intracranial DWI studies, predominantly in glioblastoma and gliomas1, have incorporated the intravoxel incoherent motion (IVIM) concept2, and demonstrated its potential for providing parameters reflecting cerebral blood volume (CBV) and perfusion without the use of intravenous contrast agent. The original IVIM concept relies on bi-exponential DWI signal decay, and accurate estimation of perfusion parameters requires image acquisition with a large number of b values3. In our study, we used a simplified model with asymptotic fitting, essentially requiring no more than three b values, to estimate cerebral blood volume4, CBVDWI, in metastases from lung cancer and normal brain tissue. The CBVDWI was compared with conventional perfusion parameters obtained from Dynamic Susceptibility Contrast (DSC) Magnetic Resonance Imaging (MRI).METHODS
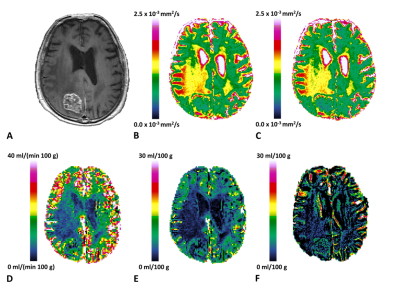
Twenty-three untreated brain metastases in 19 patients with primary non-small cell lung cancer have been included in this prospective study so far. DWI and DSC MRI were performed on a 3T scanner. DWI was acquired in three orthogonal directions with four b values: 0, 200, 300 and 1000 s/mm2 (TR/TE=5960/71 ms, voxel size = 1.22 x 1.22 mm2). A single region of interest (ROI) was manually placed separately on the DWI and DSC images in normal gray matter and white matter, and within tumor tissue in the image slice showing the greatest extent of solid tumor. The placement of ROIs was guided by co-registered high-resolution 3D isotropic T1w post-contrast images. Median DWI signal intensity within each ROI was used for estimation of the diffusion coefficient, Dlinear, and the perfusion fraction, flinear, which was subsequently used for calculation of CBVDWI as previously reported4. Post-processing of DSC spin-echo data provided maps of CBVDSC and CBFDSC5. Image analysis was performed in nordicICE and in the Interactive Data Language.RESULTS
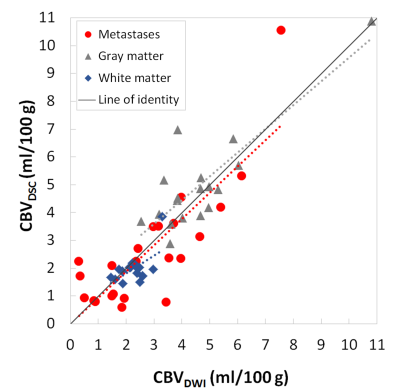
Table 1 shows median values (range) of DWI and DSC metrics from ROIs within metastases and normal brain tissue. Maps of these metrics are shown in Fig. 1. Gray matter was characterized by higher blood volume and blood flow than white matter (p<0.01). There was a strong positive correlation between CBVDWI and CBVDSC (Fig. 2) in metastases (Spearman’s ρ correlation; 0.739, p<0.01) and gray matter (Spearman’s ρ correlation; 0.633, p < 0.01). No significant correlation was however found for these parameters in white matter (Spearman’s ρ; 0.311). CBVDWI correlated with CBFDSC (Spearman’s ρ; 0.482, p<0.05), but weaker than for CBVDSC and CBFDSC (Spearman’s ρ; 0.623, p<0.05).DISCUSSION AND CONCLUSION
In our study, we show that asymptotic fitting of DWI signal decay in brain metastases from lung cancer and normal gray matter yields an estimation of cerebral blood volume that strongly correlates with blood volume obtained from conventional DSC MRI. The lack of correlation between CBVDWI and CBVDSC in white matter may be due to the inherently low blood volume of white matter. Similarly, lower agreement between CBVDWI and CBVDSC is seen in metastases with low cerebral blood volume. IVIM may serve as an independent and reliable surrogate marker of blood volume in well perfused brain tissue in the absence of contrast-enhanced MRI.Acknowledgements
No acknowledgement found.References
- Puig et al, PloS One 2016;11(7):e0158887
- Le Bihan et al, Radiology 1988;168:497-505
- lima M et al, Invest Radiol 2014;49(7):485-90
- Wirestam et al, Acta Radiol. 2001;42(2):123-8
- Bjornerud A et al, JCBFM 2010;30(5):1066-78
Figures
*CBVDWI = flinearxFw/ρ (FW=0.65: MR visible water content fraction of tissue, ρ=1.047: Tissue density)
**For one patient, placement of ROIs in gray matter and white matter was hampered by a combination motion, multiple metastases and large regions of edema.