3805
Practical Aspects of MRI-based Gel Dosimetry in RT Quality Assurance1CR-UK and EPSRC Cancer Imaging Centre, Royal Marsden NHS Foundation Trust & Institute of Cancer Research, Sutton, Surrey, United Kingdom, 2Radiotherapy, Royal Marsden NHS Foundation Trust, London, United Kingdom, 3Technological Educational Institute of Athens, Department of Radiology-Radiotherapy, Athens, Greece
Synopsis
MRI-based gel dosimetry has been proposed as a part of a Radiotherapy QA programme and is of interest to Stereotactic Ablative Radiotherapy and Stereotactic Radiosurgery. MRI-related sources of error that may compromise the dosimetric accuracy need to be considered. R2 measurement variations associated with measurement timing after irradiation and SAR limitations were investigated using an anthropomorphic head phantom. Our results demonstrate gradual gel deformation and R2 variations that could have an impact on relative and absolute dose measurements.
Introduction
MRI-based gel dosimetry is of great interest to Stereotactic Ablative Radiotherapy (SABR) and Stereotactic Radiosurgery (SRS) quality assurance (QA)1,2,3; these procedures deliver the dose in very few fractions and therefore demand high accuracy4.
In this work we investigate potential sources of errors associated with practical aspects of MRI measurements for gel dosimetry. We employ a commercial anthropomorphic head phantom5 and a complex treatment plan delivering high doses with different IGRT systems. We consider the accuracy and the stability of measurements of relaxation times, and how they impact on relative and absolute dose measurements.
Methods
Two identical anthropomorphic head phantoms were 3D-printed from a clinical CT dataset (RTSafe5). One phantom contained radiosensitive gel held in the cranial cavity, and the other contained ionisation chambers for direct dose measurements using conventional methods5. A RT plan was produced as if to irradiate three different spheroid metastatic lesions (large-5.4cc, medium-0.75cc and small-0.15cc), separated by at least 50mm.
MRI scanning was performed at 1.5T using a standardized RT positioning for head/neck. A 2D-fast spin-echo sequence with multiple echo times was employed (TR/TE=2000ms/36,436,835,230ms, voxel size=1.4x1.4x2mm3, bandwidth=780Hz/px. In addition to the MRI-scan recommended by RTSafe (within 48h of irradiation–post1), we also performed scans before irradiation and at later time points: one week (post2) and one month (post3) post-irradiation.
The R2 uniformity of the gel pre-irradiation was evaluated. Knowing that R2 measurements with fast spin-echo sequences require high SAR levels, we investigated the effects of flip angle reduction on the accuracy of R2, performing measurements with flip angles 130° and 111°. The stability of the R2 measurements over time and the direct relationship between R2 and applied dose was also investigated. We considered both MR-CT co-registration of the entire test object and local co-registration of smaller regions centred on each lesion (3DSlicer, 4.6.2) to detect deformations. The difference in the R2-dose response was explored for 3 different regions of interest (ROIs) encompassing each lesion. MR-CT co-registration of the entire test object was used for this comparison.
Results
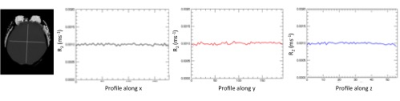
Pre-irradiation measurements demonstrated the uniformity of the gel within the phantom; no drifts were observed and R2 variations were simply attributed to noise (Figure 1). The average R2 before irradiation is 0.00100±0.00002 ms-1.
Due to high SAR it was necessary to reduce the spin-echo flip angle to 130° to keep the measurement within a reasonable time. Reducing the flip angles, significantly reduced R2 values for all three lesions (p<0.05, Mann-Whitney U test). The largest variation occurred for the largest lesion (6%).
On all areas receiving high doses, post2 and post3 R2 exhibited an increase (13% and 19%, respectively) when compared to post1 R2 (a day after irradiation) (Figure 2), suggesting gradual changes to the polymer gel post-irradiation. In addition, it was possible to detect gel deformation a month after irradiation (post3). Localised co-registration of each lesion suggests that shifts of up to 2mm may have occurred.
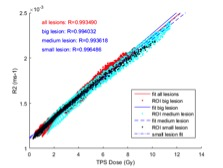
Dose-R2 response from all ROIs and each ROI separately are shown in Figure 4. For a fixed value of R2 of 2.2E-3 ms-1 a dose difference of ~2.5%, 3.3% and 1.2% was obtained for the large, medium and small ROIs respectively, compared to the data from all ROIs.
Ionisation chamber measurements revealed small average percentage error in dose for all image-guided RT systems (<2.2%). Highest error occurred for the smallest lesion (4.0% in average).
Discussion and conclusion
Gel dosimetry with anthropomorphic phantom is a very attractive end-to-end QA tool. Our work supports the manufacturer’s advice for the timing of the measurements. Later measurements presented discrepancies in R2 values and test object geometry, relevant to the accuracy of the system. SAR limitations may also compromise the dosimetric accuracy. A 6% change in R2 would result in approximately 1Gy dose change.
Absolute dose measurements using the ionisation chambers demonstrated the technical accuracy of our methods. Small differences in dose-R2 response were found between the different lesions. The higher variations for the medium lesion may relate to registration errors. Different dose-R2 response may also be caused by different dose levels within each ROI (large lesion only up to 9Gy) (Figure 4). This variation creates uncertainties in the definition of the dose normalisation point, which could under- or over-estimate DVH values.
This work demonstrates an approximately linear relationship between dose and R2. This behaviour is well-suited to relative localised dosimetric measurements, invaluable to the assessment of complex RT plans. However, protocol standardisation in gel-MRI dosimetry is a prerequisite and further refinement is necessary before absolute dose values can be derived from gel alone.
Acknowledgements
CRUK and EPSRC in association with MRC, NHS funding Biomedical Research Centre and Clinical Facility in Imaging.References
1. Liu H et al. Dosimetric validation for an automatic brain metastases planning software using single-isocenter dynamic conformal arcs. J Appl Clin Med Phys. 2016; 17: 142-156
2. Pappas E. et al. Narrow stereotactic beam profile measurements using N-vinylpyrrolidone bases polymer gels and magnetic resonance imaging. Phys Med Biol 2001; 46:783-797.
3. A new polymer gel for magnetic resonance imaging (MRI) radiation dosimetry. E Pappas, T Maris, A Angelopoulos, M Paparigopoulou, L Sakelliou, P Sandilos, S Voyiatzi and L Vlachos. 1999 Phys. Med. Biol. 44 2677 (http://iopscience.iop.org/0031-9155/44/10/320) www.rt-safe.com
4. National Radiotherapy Implementation Group Report; Stereotactic Body Radiotherapy; Guidelines for Commissioners, Providers and Clinicians in England 2011
5. http://www.rt-safe.com/
Figures