3784
Development and Evaluation of a contrast optimized 3D SHINKEI MR Neurography on patients with Brachial plexus injuries at 1.5T1Radiodiagnosis and Imaging, Kasturba Medical College, Manipal, India, 2Philips India, Bangalore, India, 3Philips India, Gurugram, India
Synopsis
The objective of this work is to optimize the 3D nerve-SHeath signal increased with INKed rest-tissue RARE Imaging (SHINKEI) sequence for the best nerve-muscle T2 contrast in 1.5T and evaluate the clinical feasibility of this optimized sequence in 24 patients with brachial plexus injuries. Based on the evaluation by two experienced radiologists and the comparison to surgical observations, the optimized SHINKEI sequence performed better than fat suppressed TSE (STIR TSE) and Diffusion Weighted Imaging with Background Suppression (DWIBS) sequences that are currently widely used in the clinical protocols
Introduction
Brachial Plexus is a group of peripheral nerves that innervates the muscles of the upper extremities. It is an injury prone anatomy which can be involved in a variety of pathologies leading to impaired upper limb functions. Hence there is considerable interest to develop robust imaging techniques; however the complicated anatomy makes it extremely difficult to image. Fat suppressed Inversion Recovery Turbo Spin Echo(1) (Ex: STIR TSE) and Diffusion Weighted Imaging with Background signal Suppression (DWIBS(2)) based MR Neurography sequences are commonly employed sequences to visualize brachial plexus. 3D nerve-SHeath signal increased with INKed rest-tissue RARE Imaging (3D SHINKEI) is a recently introduced MRN sequence that is used to visualize brachial plexus. The goal of this study is to develop a nerve-muscle contrast optimized 3D nerve SHeath signal increased with INKed rest-tissue RARE Imaging (3D SHINKEI(3,4)), sequence and to evaluate its clinical feasibility for imaging the brachial plexus at 1.5T.Methods
Institutional Ethical Committee (IEC) approval was obtained for this prospective study. All experiments were performed on a 1.5 T MR Scanner (Achieva, Philips, Best, The Netherlands)
Sequence Optimization
The T2 preparation duration of Improved Motion Sensitized Driven Equilibrium (iMSDE) module of the SHINKEI sequence was optimized to provide a higher nerve signal and an improved nerve-muscle contrast resolution (CR) on a 1.5 T scanner using the following equations.
S = exp(-T2prep/T2)
Cnerve-muscle = (Snerve - Smuscle)/ (Snerve + Smuscle)
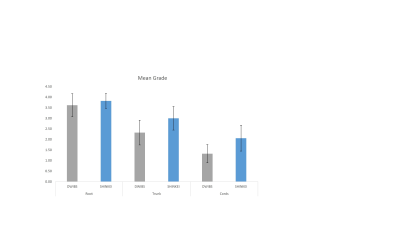
This optimized sequence was evaluated on seventeen healthy volunteers, and was compared to the clinically widely used DWIBS Neurography sequence. The visualization of root, trunk and cord of the brachial plexus obtained from these two sequences was rated on a four-point scale by a panel of two experienced radiologists and compared using Wilcoxon signed Rank test.
Clinical feasibility Study
On conclusion of the volunteer study, the optimized SHINKEI sequence was used to obtain data from 24 patients clinically advised for brachial plexus imaging. These data were then compared to Neurography data obtained with DWIBS and STIR TSE sequences as part of the clinical exam. The diagnostic quality of SHINKEI for different locations of brachial plexus was rated through consensus on a four-point scale by a panel of two experienced radiologists. In addition, these data were also compared to the surgical results available in seven of the 24 patients. Chi square test was performed to compare the predictive potential of SHINKEI, STIR TSE and DWIBS in this regard.
Results
Sequence Optimization
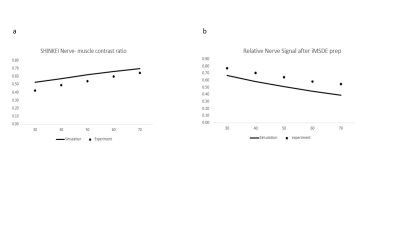
Based on the results obtained from the optimization, a T2 prep duration of 50 milliseconds was concluded as the optimal duration at 1.5T that provides a satisfactory nerve signal and an improved nerve-muscle contrast resolution (fig. 1). Figure 2 shows that the trunks and cords of the brachial plexus were better visualized with the optimized SHINKEI compared to DWIBS (p = 0.002 for both cases) as opposed to the roots of the plexus which showed no significant improvement in visualization (p>0.05).
Clinical Feasibility
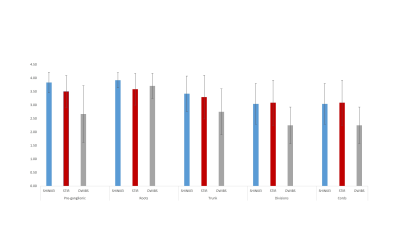
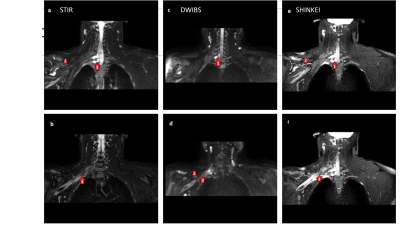
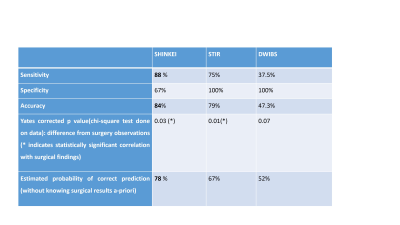
Figure 3 shows the comparison of the clinical data obtained with the three sequences; the mean scores obtained from the optimized SHINKEI were typically much better than the data obtained with DWIBs. Compared to STIR TSE, the visualization of the proximal parts of the plexus, preganglionic and post ganglionic roots was statistically better with SHINKEI (p =0.02) however there was no significant difference in the visualization of distal parts. The division and cords are visualized better with SHINKEI compared to DWIBS (p <0.001) There is no difference in the way the roots are visualized Fig 1: SHINKEI shows the grade 1 hyper intensity on the fine nerves structure better than the STIR TSE and DWIBS ((arrow marked 2). Nineteen nerve roots were identified in surgery from the seven patients. The results compared with the predictions from the 3 sequences are displayed in table 1.
Discussion
The visualization of brachial plexus anatomy is superior with the optimized SHINKEI sequence than the DWIBS sequence. There is significant correlation in the outcomes predicted by SHINKEI and the surgical findings. SHINKEI sequence could be employed with greater confidence in the detection proximal plexus injuries compared to 2D STIR TSE as a rule out mechanism owing to its higher sensitivity and hence possibly SHINKEI could be a better predictive tool prior to surgical planning.Conclusion
Based on the clinical feasibility data performed in this study, we conclude that the optimized SHINKEI sequence is a potential candidate MR sequence to improve decision making for imaging the brachial plexus and warrants investigation on a larger patient cohort.Acknowledgements
No acknowledgement found.References
1. Yoneyama M, Nakamura M, Okuaki T, Tabuchi T, Takemura A, Obara M, et al. High Resolution 3D Volumetric NerveSheath Weighted RARE Imaging. In: Proceedings of International Society of Magnetic Resonance in Medicine. Cubec, Canada; 2011.
2. Yoneyama M, Takahara T, Kwee TC, Nakamura M, Tabuchi T. Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci MRMS Off J Jpn Soc Magn Reson Med. 2013;12(2):111–9.
3. Kasper JM, Wadhwa V, Scott KM, Rozen S, Xi Y, Chhabra A. SHINKEI—a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. Eur Radiol. 2015 Jun;25(6):1672–7.
4. Chhabra A, Andreisek G, Soldatos T, Wang KC, Flammang AJ, Belzberg AJ, et al. MR Neurography: Past, Present, and Future. Am J Roentgenol. 2011 Sep;197(3):583–91.
Figures