3741
Diffusion Kurtosis Imaging of the Motor Cortex in Amyotrophic Lateral Sclerosis1Sydney Translational Imaging Laboratory, University of Sydney, Sydney, Australia, 2GE Healthcare, Richmond, Australia, 3GE Healthcare, Palo Alto, CA, United States, 4GE Healthcare, Calgary, AB, Canada, 5GE Global Research, Niskayuna, NY, United States, 6MND Research Centre, Sydney, Australia, 7Department of Radiology, Royal Prince Alfred Hospital, Sydney, Australia
Synopsis
Amyotrophic lateral sclerosis (ALS) is characterised by degeneration of the motor neurons. Diffusion kurtosis imaging (DKI) may be a suitable biomarker for neuronal injury in ALS. We imaged 30 people with ALS and 63 controls with a 140-direction DKI protocol and explored group differences diffusion and kurtosis scalar values within the motor cortex. Our preliminary data show that significant microstructural changes are measurable by DKI in people with early ALS. DKI may represent a viable biomarker of early ALS progression.
Introduction
Amyotrophic lateral sclerosis (ALS) is a degenerative disorder of the motor neurons. Current methods for diagnosis are based on clinical signs and are insensitive during early disease stages when the potential for treatment benefit is greatest. Earlier detection of pathobiology is therefore critical for enabling timely clinical management and trial enrolment.
Diffusion kurtosis imaging (DKI) uses multiple b-values to model the non-Gaussianity of diffusion in anisotropic media. DKI may act as a sensitive biomarker of neuronal injury which, coupled with multi-slice acceleration, is feasible for clinical translation. We hypothesised that abnormalities in DKI scalars in the motor cortex would reflect the severity of ALS pathological progression.
Methods
We performed magnetic resonance imaging (MRI) on 30 people with clinically-definite ALS within 24 months of diagnosis (average 17±6 months) and 63 healthy controls using an optimised DKI protocol on a 3T GE Discovery MR750w scanner with a 32-channel Nova head coil. The sequence was a multi-shell multi-band diffusion MRI with a phase offset applied to each multi-band component and a reversed phase-encode correction: 140 unique gradient directions (b-values 700, 1000 and 2800) and eight interleaved b=0 volumes, TR 3245ms, TE 100ms, flip angle 90°, matrix 128x128, 66 slices, voxel dimensions 1.875x1.875x2.5mm, FOV 240mm, scan time 9 minutes. Clinical evaluations for disease severity were made using the ALS functional rating scale (ALSFRS-R). A T1-weighted MPRAGE-PROMO was also acquired for anatomical parcellation. The motor cortex was segmented using FreeSurfer and registered to a b=0 volume. The mean values of DKI scalars in the mask were evaluated for group differences and relationships to severity. We focussed on the following diffusion and corresponding kurtosis scalars: apparent diffusion coefficient (ADC), apparent kurtosis coefficient (AKC), fractional anisotropy (FA), FA of kurtosis (FAK), axial diffusivity (AD), axial kurtosis (AK), radial diffusivity (RD), radial kurtosis (RK), mean diffusivity (MD) and mean kurtosis (MK).Results
Groups were matched for age (p=0.142) and sex (p=0.483). The ALS group had significantly reduced motor cortex thickness and volume (percentage difference in ALS group; left volume -8.4%, p=0.018; left thickness -4.5%, p=0.006; right volume -8.5%, p=0.023; right thickness -4.3%, p=0.010). Whole-brain volume, intra-cranial volume and brain parenchymal fraction were not significantly different. ALSFRS-R scores at baseline indicated mild-to-moderate disability 35±11 (out of 48; higher meaning less impairment).
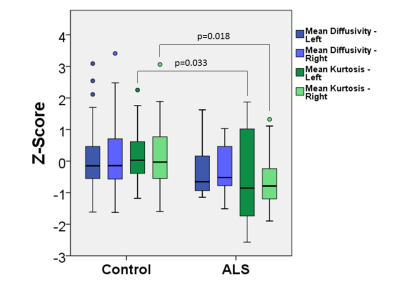
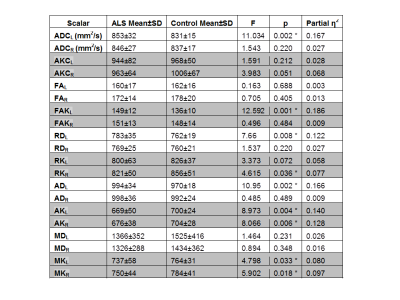
Significant group differences were observed for a number of diffusion and kurtosis scalars in the motor cortex (multivariate GLM controlling for age; Table 1). Figure 1 highlights group differences in MD and MK, and contrasts the two scalars. Significant correlations with disease severity were observed for FAK and AD in the right hemisphere only, (Pearson correlation; FAKR, r=-0.853, p=0.007; ADR, r=-0.824, p=0.012), although these were non-significant after multiple comparison correction
Discussion
Our findings suggest that microstructural changes are present in the motor strip in ALS and are measurable by DKI. These changes were observed in a mildly-impaired sample, indicating that DKI may be sensitive to neurodegeneration at an early stage. The observed DKI changes did not always correspond to those in conventional diffusion scalars. A possible interpretation is that of a change from an intact tissue with multiple water compartments (due to a combination of axons and cell bodies) to a disintegrated tissue with fewer distinct compartments, but without net loss of membranes. Previous studies have primarily only investigated white matter diffusion changes (Kassubek et al, 2012), so future work will look additionally at the impact of neurodegeneration in the pericortical white matter and deep white matter using DKI.
Limitations: Although unilateral presentation is typical in ALS, our analysis did not distinguish symptomatic from non-symptomatic hemispheres due to availability of clinical information. This would likely increase our measured effect considerably.
Conclusion
We find significant microstructural changes in the motor cortex in people with ALS. DKI may represent a viable biomarker of early ALS progression. Further longitudinal studies are proceeding to evaluate prognostic potential.