3737
Investigation of cognition associated cerebral perfusion changes in Alzheimer's disease and mild cognitive impairment using a novel 3D arterial spin labeling technique1GE Healthcare, Shanghai, China, 2Radiology, Ruijin Hospital, Shanghai, China, 3GE Healthcare, Beijing, China
Synopsis
This preliminary study investigated cognition associated cerebral perfusion changes in Alzheimer’s disease (AD) and mild cognitive impairment (MCI) measured with a novel 3D arterial spin labeling technique. The voxel-wise regression analysis against MMSE scores was performed using whole brain CBF maps. Cognition associated CBF deficits in the hippocampus and insular cortex might cause the typical AD symptoms including memory loss and emotion issues. CBF decrease in MCI patients in the lingual gyrus could affect vision and wording functions. CBF increase in the frontal lobe might serve as an early indicator for high-level cognitive function disturbance.
Purpose
Alzheimer’s disease (AD) and mild cognitive impairment (MCI) are among major neurodegenerative disorders for the elderly population. Recent studies revealed cerebral perfusion deficiencies in AD and MCI by making comparison against normal controls (NC).1 However, brain regions with cognition associated cerebral perfusion deficits need to be further validated. In this preliminary study, a novel pulsed-continuous 3D arterial spin labeling technique implemented with the fast spin echo (FSE) framework to minimize susceptibility artifacts and multi-shot excitation to improve the labeling efficiency was used to provide whole brain quantitative perfusion measurements.2 The Mini-Mental State Examination (MMSE), a brief 30-point questionnaire, was used to score disease relevant cognitive decline. Voxel-wise regression analysis of whole brain perfusion maps against MMSE scores were performed to detect cognition associated cerebral perfusion changes for the AD and MCI groups respectively.
Methods
All the subjects gave written informed consent to participate the study, which was approved by the local ethical committee. Ten AD patients (aged 74.6±6.7 years, 5 females) and nine MCI patients (aged 71.4±7.6 years, 4 females) were recruited according to the criteria of NINCDS-ADRDA, PADCS and MMSE scores. The MMSE scores ranged from 9 to 23 for AD patients (14.8±2.6) and from 24 to 26 for MCI patients (24.8±0.9). Perfusion scans were performed with a 3.0-T HDXT scanner (GE Healthcare, Milwaukee, WI) using an 8-channel phase array head coil. Two sets of ASL images were acquired with and without the spatially selective inversion (tagging) pulse (TR/TE 1350/5 ms, flip angle 155°, labeling duration 1.5 s, post label delay 1.5 s, matrix =128x128, FOV 24 cm, thickness/gap 4/0 mm). The difference maps between the tag and control pairs were averaged for each subject and quantitative cerebral blood flow (CBF) maps were calculated with the vender provided toolbox. Image pre-processing was performed using SPM8 (http://www.fil.ion.ucl.ac.uk/spm). Spatial transformation included a three-dimensional rigid body registration to correct for head motion, followed by a nonlinear warping to spatially normalized CBF maps into a standard stereotaxic space. The normalized CBF maps were resampled to 2x2x2 mm3 isotropic voxel size and smoothed with a 6 mm isotropic Gaussian kernel. A second-level regression analysis against MMSE scores was performed to identify cognition relevant perfusion abnormalities for the AD and MCI groups respectively. For multiple comparison correction, the AlphaSim program implemented in AFNI (http://afni.nih.gov/afni/docpdf/AlphaSim.pdf) was used to control the false positive rate (corrected p<0.05).
Results
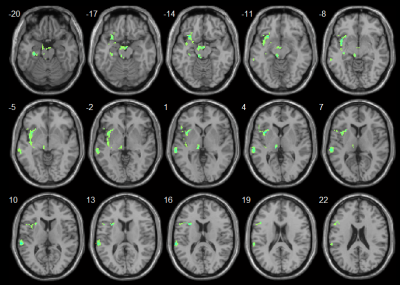
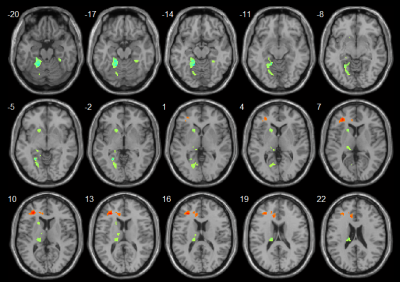
AD patients exhibited cognition associated CBF decrease in the left hippocampus, para-hippocampus, insula, middle temporal gyrus, superior temporal gyrus and thalamus (Fig. 1). MCI patients showed cognition associated CBF decrease in the left lingual gyrus, fusiform gyrus, putamen and thalamus but increased CBF in the left anterior cingulate cortex and middle frontal gyrus (Fig. 2).
Discussion and Conclusion
Both AD and MCI patients showed cognition associated CBF decrease. CBF deficits in the hippocampus, para-hippocampus and insular cortex might cause the typical symptoms of AD patients including memory loss, disorientation and emotion issues. For MCI patients, CBF decrease in the lingual gyrus could affect vision and wording functions. The abnormal CBF increase in the frontal lobe might serve as an early indicator for high-level cognitive function disturbance.
Acknowledgements
No acknowledgement found.References
1. Ding B, Lin H, Zhang Y, et al. Pattern of cerebral hyperperfusion in Alzheimer’s disease and amnestic mild cognitive impairment using voxel-based analysis of 3D arterial spin-labeling imaging: initial experience. Clinical Interventions in Aging. 2014;9:493–500.
2. Dai W, Garcia D, de Bazelaire C, et al. Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med. 2008;60(6):1488-1497.