3683
Optimization of MR-Based Attenuation Correction for Cardiac PET/MR Using Free-Breathing Multi-Echo Golden-Angle Radial Stack-of-Stars MRPhilip Robson1, Thomas Benkert2, MariaGiovanna Trivieri3, Nicolas Karakatsanis1, Ronan Abgral4, Marc Dweck5, Jason Kovacic3, Tobias Block2, and Zahi Fayad1
1Translational and Molecular Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2Center for Advanced Imaging Innovation and Research, New York University School of Medicine, New York, NY, United States, 3Cardiovascular Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 4Department of Nuclear Medicine, European University of Brittany, Brest, France, 5British Heart Foundation Centre for Cardiovascular Science, University of Edinburgh, Edinburgh, United Kingdom
Synopsis
Recently hybrid PET/MR has gained much interest for its potential to combine PET imaging of disease activity with the benefits of cardiac MR. MR-based attenuation correction (MRAC) is an important aspect of accurate PET tracer quantification. For imaging the heart, optimal MRAC is required to both compensate for cardiac motion and also to optimize segmentation of tissues for accurate PET reconstruction. In this work we investigate the use of multi-echo golden-angle radial stack-of-stars MR to combine these 2 key attributes.
Purpose
Cardiac applications of hybrid PET/MR have recently gained much attention for the power of PET/MR to combine two cardiac imaging modalities in a single scan with perfect co-registration between each data set and at lower radiation dose compared to MR plus PET/CT. Recently, it was demonstrated that attenuation correction based on breath-held MR was unsuitable for cardiac applications where difference in anatomical locations between MRAC and PET emission data introduced significant artifacts at the liver-lung and heart-lung boundaries, confounding evaluation of myocardial and coronary PET tracer uptake1. This was solved by employing a golden angle radial stack-of-stars trajectory acquired over several minutes to average respiratory motion of the heart. Attenuation maps were made by thresh-holding image intensity into 2 classes comprising 1) all soft tissue including fat and 2) background air plus lungs. The purpose of this work is to investigate the feasibility of using a multi-echo stack-of-stars sequence (DIXON-radial-VIBE) to separate water and fat based on their chemical shift whilst maintaining the benefit of motion averaging.Methods
DIXON-radial-VIBE MRAC: acquisition parameters included: FOV = 500 cm, resolution 3.1 mm isotropic, TR/FA/BW 10 ms/12o/1010 Hz/pix, TE1/TE2/TE3 1.84/3.48/5.12 ms, 384 radial views, scan time = 5:51 min. Water and fat images were decomposed using previously described methods2. Attenuation maps were then composed by masking the fat and water images. Linear attenuation coefficients (LACs) were assigned to the mask (LACwater = 0.1 cm-1, LACfat = 0.0854 cm-1). On a slice-by-slice basis, the summation of fat and water components was used as a template to extract lung, which was identified as all remaining dark space within the mask of the body and assigned the LAC of lung (LAClung = 0.0224 cm-1). All other background pixels outside the body were assigned a LAC value of zero. PET/MR Imaging: Three patients undergoing PET/MR to evaluate cardiac sarcoidosis were scanned 30 min after administration of 370 MBq (10 mCi) 18F-FDG and data acquired for 60 minutes on the Biograph mMR PET/MR system (Siemens, Erlangen). PET images were reconstructed with the 2-component attenuation map; a 3-component map with soft tissue, fat and background (lung set to background air); a 3-component map with soft tissue, lung and background (fat set to soft tissue); and a 4-component attenuation map comprising soft tissue, fat, lung and background air. Three hotspots per patient were identified, in the lateral wall, the septum, and the anterior wall. SUVmean, SUVmax and TBR (SUVs normalized to SUVmean of atrial blood) were measured on PET images using each MRAC map. Quantitative analysis of the impact of multiple tissue components on the PET image data was performed with a paired t-test between MRAC types.Results
The 4 different attenuation maps are shown in Fig. 1 along with 18F-FDG-PET and PET fused with the source DIXON-radial-VIBE image. Measured SUV and TBR values are summarized in Table 1. Myocardial SUV values were significantly lower (higher) when correctly assigning fat (lung) in the attenuation map compared to the 2-component map. TBR values were significantly higher when lung was correctly assigned, and almost reached significance using the 4-component map.Discussion and Conclusion
This work has demonstrated the feasibility of multi-echo radial MR to form MRAC attenuation maps including the tissue classes: soft tissue, fat, lung and background air, in combination with the motion averaged anatomical information from the radial trajectory during free breathing. The preliminary results presented here show that the correct assignment of fat and lung tissues in the attenuation map significantly affects tracer quantification in the heart. The effect of lung and fat are opposite which can be attributed to the fact that lung attenuation is under-estimated if assigned as air, and fat attenuation is over-estimated if assigned as soft tissue. In this data, this dichotomy has lead to a non-significant difference between simple 2-component MRAC and a more sophisticated 4-component map including fat and lung components. However, correct attenuation correction should employ 4 tissue classes to ensure robust quantitative results, which is of importance in diagnostic terms when comparing to pre-defined activity thresholds and in longitudinal studies of disease or response to therapy. The impact of pericardial fat which is close to the tissue of interest and changeable in volume between patients may have an important impact on tracer quantification in the myocardium and coronary arteries and needs to be investigated further. Moreover, this effect should now be investigated in larger cohorts of patients.Acknowledgements
This work was supported by NIH grant R01 HL071021References
1. Robson PM, Dweck MR, Trivieri MG et al. Coronary Artery PET/MR Imaging: Feasibility, Limitations, and Solutions.JACC Cardiovasc Imaging 2017 10(10):1103-12. 2. Benkert T, Feng L, Sodickson DK et al. Free-breathing volumetric fat/water separation by combining radial sampling, compressed sensing, and parallel imaging. MRM 2017;78:565-576.Figures
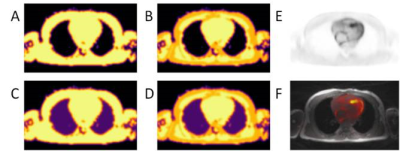
Figure 1: MRAC maps
derived from DIXON-radial-VIBE with A) 2 components: soft tissue (light yellow)
and background air (black), B) 3 components including fat (orange), C) 3
components including lung (purple) and D) 4 components. FDG-PET uptake in the myocardium (E) is fused
on free breathing radial-VIBE source image (F).
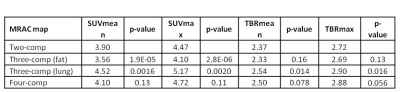
Table 1: Quantitative analysis
of PET tracer uptake: p-values of paired t-test between given MRAC map and
2-component MRAC map