3666
Is occipital bending a structural biomarker of risk for depression and sensitivity to treatment?1Department of Radiology, Royal Prince Alfred Hospital, Sydney, Australia, 2General Electric Healthcare, Richmond, Australia, 3Sydney Translational Imaging Laboratory, Heart Research Institute, University of Sydney, Sydney, Australia, 4Department of Psychiatry and Behavioural Sciences, Stanford University, Stanford, CA, United States, 5The Brain Dynamics Centre, Westmead Institute for Medical Research, University of Sydney, Sydney, Australia, 6Duke-National University of Singapore, Singapore, Singapore, 7Brain Resource Ltd, Sydney, Australia, 8Department of Psychiatry and Behavioral Sciences, Miller School of Medicine, University of Miami, Miami, FL, United States
Synopsis
Occipital Bending (OB) was investigated as an MRI imaging biomarker for major depressive disorder (MDD) using data from large, well characterized, international, randomised study recruiting non-geriatric adult participants (iSPOT-D, n=68 control, 231 MDD). The presence of OB and the angle of occipital bending (OBA) was correlated with a repeated battery of neuropsychiatric assessments, and response to 6 weeks of antidepressant treatment. A greater proportion of rightward bending was present in MDD in comparison to control individuals. Underlying association between OB and MDD is likely.
Introduction
The majority of MDD research has focused on structural and functional changes in frontal and subcortical regions of the brain. However, there is a growing body of evidence implicating the occipital lobes in the depressed brain. (e.g. 1-3) Occipital bending (OB) is an easily assessable but rarely-investigated potential MRI biomarker for major depressive disorder (MDD). OB is defined as the presence of asymmetrical twisting of one occipital pole beyond the midline and has shown strong associations across multiple psychiatric conditions including MDD, 4 bipolar depression, 5 and schizophrenia. 6 These previous studies suggest that OB is 3-4 times more prevalent in affected individuals. This study aims to validate these findings in a large, independent MDD population drawn from iSPOT-D, the international Study to Predict Optimized Treatment for Depression (iSPOT-D). 7Materials and Methods
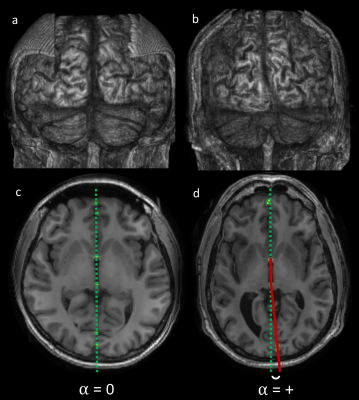
A total of 231 adult, non-geriatric participants with MDD and 68 control subjects were imaged at baseline with T1-weighted volumetric MRI. 8 Clinical status was evaluated using the Hamilton Rating Scale for Depression (HRSD17), with remission defined as HRSD17<7 at 6 weeks. Data were acquired using a 3 Tesla GE Signa Twinspeed HDx scanner (GE Healthcare, Milwaukee, Wisconsin, USA) with an 8 channel phased array head coil (1mm isotropic resolution; 256x256 matrix; TR:8.3ms; TE:3.2ms; Flip angle:11°; TI:500ms; NEX=1; ASSET=1.5). OB was assessed by two observers blinded to diagnosis, by visual inspection of a three-dimensional reconstruction of the brain, manually skull-stripped in Osirix. 9 The OB angle (OBA) was also calculated as the mean angle between the medial aspects of the occipital poles relative to the midline on a single SPGR slice representing the AC-PC line (Fig. 1). 10 Midline was delineated by the line along the third ventricle connecting the midpoint of the anterior and posterior commissures.Results
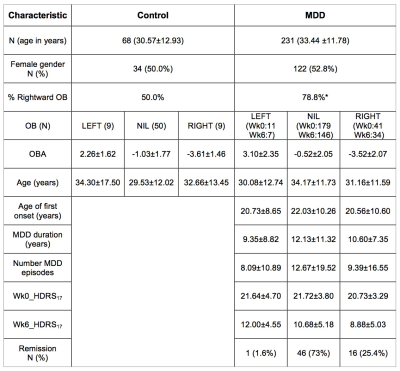
Groups were matched for age (p=0.09) and sex (p=0.14). In the MDD group, age of first onset was 21.71±10.23 years, duration of MDD was 11.72±10.61 years, and number of previous MDD episodes at 11.87±18.70. The MDD group had an average HDRS17 of 21.54±3.76 at baseline, which decreased to 10.40±5.16 at 6 weeks. A similar proportion of OB was present between MDD and control subjects (MDD with OB: n=52 (22.5%) vs control with OB: n=18 (26.5%), χ2(1)=4.59, p=0.50). However, a striking difference was seen in the proportion of leftward vs rightward OB at baseline (MDD: n=41 (17.7%) rightward and n=11 (4.8%) leftward; Control: n=9 (13.2%) rightward and n=9 (13.2%) leftward (χ2(1)=5.45, p=0.02). No relationship between OB and severity was demonstrated in the MDD group. There was a trend towards greater proportion of rightward bending in remitters in comparison to non-remitters (χ2(1)=2.88, p=0.09; Table 1). OBA was not significantly discriminative between MDD and control participants.Discussion
The proportion of MDD participants demonstrating OB is less than comparative studies (22.5% in our study in comparison to previous estimates of 35.3% in MDD 4, 34.3% in bipolar depression 5, and 35.1% in schizophrenia). 6 In contrast, control participants demonstrated greater OB than previous studies (26.5% in comparison to 12.5%, 8.3% and 13.6%). This study is higher powered than previous investigations and has been performed with a great deal of standardisation, so these numbers likely represent a better estimate of the true prevalence of OB in normal individuals and in outpatient depression. The iSPOT-D participants are derived from a relatively young population, and are clinically moderately severe, which may also explain the lower rate of OB in our study. The underlying causation of OB remains unclear. Hypotheses include incomplete neural pruning during neuronal development, underlying white matter dysfunction or relative asymmetry of ventricular size.Conclusion
Rightwards OB is seen at greater frequency in MDD participants. A weak association between direction of OB and remission is also demonstrated. Further work is justified investigating OB as a clinical marker for MDD, and elucidating the underlying pathophysiological mechanism.
Acknowledgements
We acknowledge Brain Resource as the sponsor for the iSPOT-D study (NCT00693849).
Claire Day and Catherine King are thanked as Global Study Co-ordinators
Dr Anthony Harris and Dr Tim Usherwood are thanked for their roles, as PI and co-PI, in supervision of clinical imaging evaluations and in overseeing the partnership with primary care practitioners and recruitment of patients from primary care settings.
Dr Lavier Gomes, Ms Sheryl Foster and the Department of Radiology at Westmead are thanked for their involvement in MRI data acquisition.
SMG acknowledges the support of the Sydney Medical School Foundation.
References
1. Liao Y, et al. Is depression a disconnection syndrome? Meta-analysis of diffusion tensor imaging studies in patients with MDD. J Psychiatry Neurosci. 2013;38(1):49-56.
2. Kostic M, et al. The cumulative effect of genetic polymorphisms on depression and brain structural integrity. Hum Brain Mapp. 2016;37(6):2173-84.
3. Chen Z, et al. High-field magnetic resonance imaging of structural alterations in first-episode, drug-naive patients with major depressive disorder. Transl Psychiatry. 2016;6(11):e942.
4. Maller JJ, et al. Occipital bending in depression. Brain. 2014;137(Pt 6):1830-7.
5. Maller JJ, et al. Occipital bending (Yakovlevian torque) in bipolar depression. Psychiatry Res. 2015;231(1):8-14.
6. Maller JJ, et al. Occipital bending in schizophrenia. Aust N Z J Psychiatry. 2017;51(1):32-41.
7. Williams LM, et al. International Study to Predict Optimized Treatment for Depression (iSPOT-D), a randomized clinical trial: rationale and protocol. Trials. 2011;12:4.
8. Grieve SM, et al. Brain imaging predictors and the international study to predict optimized treatment for depression: study protocol for a randomized controlled trial. Trials. 2013;14:224.
9. Rosset A, Spadola L and Ratib O. OsiriX: an open-source software for navigating in multidimensional DICOM images. J Digit Imaging. 2004;17(3):205-16.
10. Weiss KL, et al. Clinical brain MR imaging prescriptions in Talairach space: technologist- and computer-driven methods. AJNR Am J Neuroradiol 2003;24(5):922-9.
Figures