3642
Neuromelanin sensitive MRI features of substantia nigra and locus coeruleus in de novo Parkinson’s disease and its phenotypes1Neurology, Zhongshan Hospital, Fudan University, Shanghai, China, 2Radiology, Zhongshan Hospital, Fudan University, Shanghai, China, 3Shanghai Medical Imaging Institute, Shanghai, China, 4GE Healthcare, Shanghai, China
Synopsis
This current study provides in vivo evidence that width and high signal were significantly decreased in SNc and LC of de novo PD patients using NM-MRI, compared with controls. We also observed that the neuromelanin changes in substantia nigra were across both motor phenotypic expressions and non-motor (with vs. without depressive symptoms) subtypes, while LC neuron reduction is more notable in PD with depressive symptoms. Our finding implies that the NM-MR imaging have potential applications to improve the clinical diagnosis and detect the heterogeneityof PD.
Purpose
Parkinson's disease (PD) is one of the most common neurodegenerative diseases characterized by the loss of the dopaminergic neurons in the substantia nigra of the midbrain. Pathological changes in the substantia nigra (SN) and locus coeruleus (LC) occur in the early, even pre-clinical stage of PD1.Neuromelanin of the brainstem that is considered as a marker of neurodegeneration in PD can be detected by T1-weighted neuromelanin-sensitive MR images (NM-MRI)2. Here, we aim to investigate NM-MRI features of de novo PD and whether these features associate with motor and non-motor symptoms in de novo PD patients.Methods
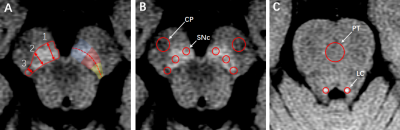
All the subjects were given written informed consent to participate in the study, which was approved by the local ethical committee. Fifty-one de novo PD patients (aged 63.90±9.91 years, 26 females) and 28 age- and gender-matched healthy control subjects (aged 63.43±7.57 years, 10 females) were recruited for group comparison. All the subjects underwent clinical examination, motor, cognitive and depression evaluations. PD patients were divided into three subgroups according to their motor phenotypes: primarily rigidity and bradykinesia with minimal tremor (PDAR subgroup); primarily tremor with minimal bradykinesia and rigidity (PDT subgroup); and mixed classic motor symptoms(PDM subgroup). Based on the cutoff score of the GDS, subjects were divided into PD with depressive symptoms (PDd) and PD with non-depressive symptoms (PDnd) subgroups. All MR data were acquired by means of a 3-Tesla MR unit (Discovery™ MR750, GE Healthcare, Milwaukee, WI). T1-weighted fast spin-echo sequence was applied to neuromelanin sensitive MRI with the following parameters: TR/TE, 600/13 ms; echo train length, 2; section thickness, 2.5 mm with no intersection gap;16 slices; matrix size, 512 × 320; field of view (FOV),220 mm; NEX, 5; and acquisition time, 8.03 min. All the NM-MR images were transferred to an AW4.6 workstation for further assessment. High signal in SN could be visible in three contiguous slices and only the middle slice, the greatest area of SN, was measured. In this slice, high signal intensity of SNc was defined following the maximal longitudinal length line which was divided into three equal segments defined as the lateral, central, and medial SNc parts. In order to assess the morphological and signal changes of SNc, we used width and the contrast-to-noise ratio(CNR) to evaluate the SNc(Fig.1).Results
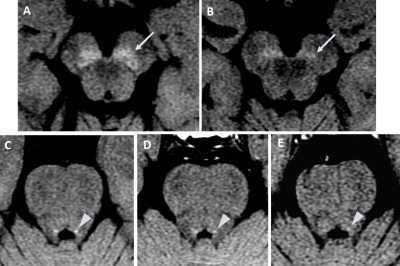
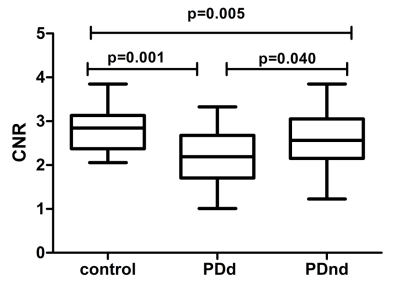
Both width and CNR values of the high signal intensity in SNc were significantly decreased in the lateral, central and medial SNc parts in de novo PD patients, when compared with control subjects(Fig.2). Significant weak correlation was only observed between the average width of contralateral substantia nigra and the lateralized UPDRS motor score from the clinically most affected side in PD patients(r=-0.289,p=0.040).The changes of SNc on NM-MRI did not show significant difference among motor subgroups. The CNR values of left LC were significant lower in the PD group than those in control group. Specifically, the subtype of PD patients with depressive symptoms exhibited significantly lowered CNR in left LC as compared with control group and PD patients without depressive symptoms (Fig.3).
Discussion and Conclusion
Substantia nigra neuromelanin changes are across both motor and non-motor (with and without depressive symptoms) subtypes, while LC changes are more notable in PD with depressive symptoms. Our results may provide new evidence to understand the pathophysiology of non-motor symptoms in de novo PD.Acknowledgements
No acknowledgement found.References
1. Braak H, Del Tredici K, Rub U, et al. Neurobiol Aging. 2003 24: 197-211.
2. Sasaki M, Shibata E, Tohyama K, et al. Neuroreport. 2006 17: 1215-1218
Figures