3615
Paravermal sign: new MR imaging features of cerebellum in neuronal intranuclear inclusion disease1Radiology, National Center of Neurology and Psychiatry, Tokyo, Japan, 2Neurology, Ciba University, Chiba, Japan, 3National Center of Neurology and Psychiatry, Tokyo, Japan
Synopsis
Neuronal intranuclear inclusion disease (NIID) is a neurodegenerative disorder with characteristic high signals along the corticomedullary junction on MR DWI. However, cerebellar findings have not been fully evaluated on MRI and we reviewed them in a series of ten NIID patients. MRI results showed cerebellar atrophy (10/10), high intensity signal on FLAIR images in medial part of the cerebellar hemisphere immediately beside the vermis (paravermal area) (7/10), and in the middle cerebellar peduncle (6/10). The paravermal abnormal signals could be a clue for diagnosis of NIID even in the past MR studies in which DWI was not examined.
Background: Neuronal intranuclear inclusion disease (NIID) is a neurodegenerative disorder, pathologically characterized by eosinophilic hyaline intranuclear inclusion in the central and peripheral nervous system, and also in the visceral organs. Recent reports have also found a finding of brain MR imaging, high intensity signal along corticomedullary junction on DWI, to be a strong clue for ante-mortem diagnosis of NIID. On the other hand, the MR imaging finding of cerebellum in patients with NIID has not been fully evaluated until today. Recently, we have experienced some cases in which abnormal signals distributed in the characteristic regions of the cerebellum on brain MR images. Herein, we present MR imaging findings focusing on cerebellum in ten patients with adult-onset NIID.
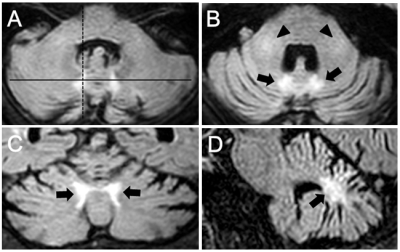
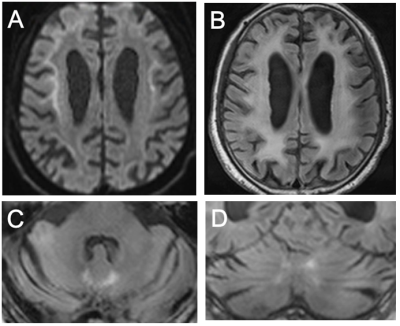
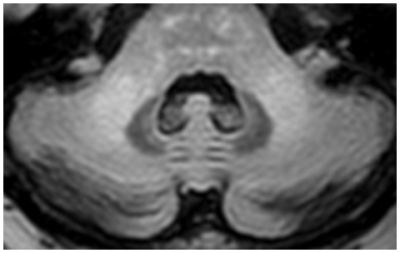
Methods: This retrospective study was approved by our institutional review board. The diagnosis of NIID was made histopathologically by skin biopsy. The medical records of the ten patients were reviewed for the history, neurological examination, executive function tests, and CSF results. All MR imaging was performed in routine clinical care by use of 1.5T scanning in 3 cases and 3T scanning in 7 cases. DWI and FLAIR images were available in all patients. The MR data in each patient were retrospectively evaluated separately and then jointly by 2 neuroradiologists. We evaluated the following findings: 1) high intensity signal along corticomedullary junction on DWI, 2) diffuse high signals of cerebral white matter on FLAIR images, 3) atrophy of the cerebellum, 4) high intensity signal in medial part of the cerebellar hemisphere immediately beside the vermis (“paravermal area”) on FLAIR images (Figure 1), 5) high intensity signal in the middle cerebellar peduncle on FLAIR images (Figure 1B).
Results: Skin biopsy was enforced in all patients. Light microscopy showed eosinophilic ubiquitin-positive and p62-positive intranuclear inclusions in the adipocytes, fibroblasts, and sweat gland cells. Electron microscopy was examined in all cases except for one and revealed dense filament material without a limiting membrane. The most common symptoms were dementia and ataxia, which were observed in 50.0 % indivisually. In all cases, the deep tendon reflex was reduced or disappeared. CSF examination showed an elevated protein in all cases. MR imaging showed high intensity signal along the corticomedullary junction on DWI, diffuse high signals of cerebral white matter and cerebellar atrophy on FLAIR images in all cases (Figure 2). Seven of 10 patients (70.0 %) showed abnormal FLAIR high signals in the paravermal area (Figures 1 and 2). Six of 10 patients (60.0 %) showed high intensity signal in the middle cerebellar peduncle (Figures 1 and 3).
Discussions: We presented characteristic MR imaging features of the cerebellum in pathologically confirmed adult-onset NIID. The abnormal FLAIR high signals in the paravermal area and in the middle cerebellar peduncle were useful MR imaging findings for diagnosing NIID. To the best of our knowledge, this is the first report that reviews MR imaging findings of cerebellum in patients with NIID. Previous studies have shown that remarkable diffuse high signals of the cerebral white matter and DWI high intensity signal along the corticomedullary junction are characteristic MR imaging findings of NIID patients. Especially, it is suggested that the finding of DWI high intensity signal along the corticomedullary junction can be a strong clue for the diagnosis of NIID. Although MR imaging findings of the cerebellum in NIID patients have not been fully evaluated, atrophy of the cerebellum has been described in several reports. In our study, we also observed cerebellar atrophy in all patients. In addition to that, we also identified abnormal signals in the medial part of cerebellar hemisphere immediately beside the vermis (paravermal area) and middle cerebellar peduncle in 70% and 60% individually. Although the latter MR finding has been reported in other diseases, such as fragile X-associated tremor/ataxia syndrome or Erdheim-Chester disease, the former one has not been detected until now. The paravermal sign might be specific finding for NIID and it could be a trigger for diagnosis of NIID, even in the past MR images in which DWI was not examined.
Acknowledgements
No acknowledgement found.References
1. Sone J, Kitagawa N, Sugawara E, et al. Neuronal intranuclear inclusion disease cases with leukoencephalopathy diagnosed via skin biopsy. J Neurol Neurosurg Psychiatry 2014; 85: 354-356.
2. Sone J, Mori K, Inagaki T, et al. Clinicopathological features of adult-onset neuronal intranuclear inclusion disease. Brain 2016; 139:3170-3186.
3. Sloane AE, Becker LE, Ang LC, et al. Neuronal intranuclear hyaline inclusion disease with progressive cerebellar ataxia. Pediatr Neurol 1994; 10: 61-66.
4. Zannolli R, Gilman S, Rossi S, et al. Herediatry neuronal intranuclear inclusion disease with autonomic failure and cerebellar degeneration. Arch Neurol 2002; 59: 1319-1326.
Figures