3577
First-pass Perfusion MRI of Myocardial Infarction Using a Novel Manganese Chelate Contrast Agent in a Rabbit Model1Department of Radiology, West China Second University Hospital, Sichuan University, Chengdu, China, 2Department of Radiology, West China Hospital, Sichuan University, Chengdu, China
Synopsis
First-pass perfusion MRI allows evaluation of myocardial perfusion in myocardial infarction (MI). While Gd3+-based contrast agents are incompatible with renal compromise, we designed and synthesized a novel manganese (Mn2+ ) based contrast agents. MI was induced in 4 rabbits, Mn2+ based and Gd3+-based first-pass perfusion MRI were performed on a 3.0T MRI scanner. All rabbits survived without significant differences in heart rate and left ventricular function. All the perfusion parameters of infarcted and normal myocardial segments correlated well between Gd-based and Mn-based perfusion imaging. Our novel Mn2+ contrast agents is safe and reliable to visualize myocardial perfusion in MI.
Synopsis
First-pass perfusion MRI allows evaluation of myocardial perfusion in myocardial infarction (MI). While Gd3+-based contrast agents are incompatible with renal compromise, we designed and synthesized a novel manganese (Mn2+ ) based contrast agents. MI was induced in 4 rabbits, Mn2+ based and Gd3+-based first-pass perfusion MRI were performed on a 3.0T MRI scanner. All rabbits survived without significant differences in heart rate and left ventricular function. All the perfusion parameters of infarcted and normal myocardial segments correlated well between Gd-based and Mn-based perfusion imaging. Our novel Mn2+ contrast agents is safe and reliable to visualize myocardial perfusion in MI.Introduction
Cardiac MRI has been considered an important multi-modal imaging method for non-invasive assessment of myocardial infarction, especially with application of Gadolinium (Gd3+)-based contrast agent. First-pass perfusion MRI allows non-invasive evaluation of myocardial perfusion and semi-quantification of perfusion parameter according to AHA segmentation1. While Gd-based contrast agents are incompatible with renal compromise, nearly 20% of MI patients cannot benefit from Gd-based imaging2,3. The limitation underscores the need for safe alternative contrast agent. We designed and synthesized an aza-semi-crown pentadentate chelator that formed manganese (Mn2+ ) complexes as a novel MRI contrast agent4. The aim of the present study was to evaluate the feasibility of novel Mn2+ chelate to quantify myocardial perfusion in myocardial infarction, by comparison with Gd-based First-pass perfusion MRI.Methods
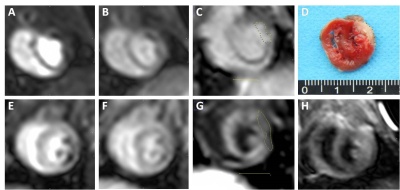
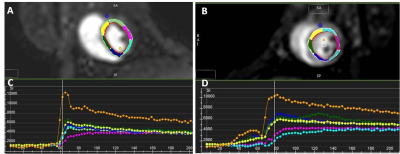
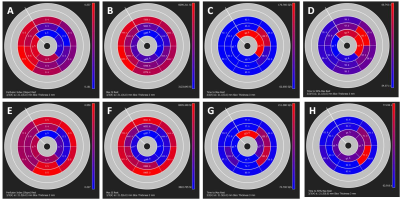
MI was induced in 4 rabbits by permanent occlusion of left circumflex coronary artery. After 7days post-surgery, cine MRI, T1WI, T2WI, first-pass perfusion MRI and delayed enhancement MRI were performed on a 3.0T clinical MRI scanner (Achieva, Philips, Andover, MA) with a clinical 8-channel knee coil. Dynamic signal changes on first-pass perfusion MRI was acquired using segmented turbo-FLASH sequence with 80 dynamic acquisitions. Three contiguous short-axis images was obtained after intravenous injection of gadolium (Gd-DTPA, Magnevist, Berlin, Germany) at 0.15 mmol/kg and Mn2+ chelate successively. A 120-minute washout period proceeded between DEMRI and MEMRI to ensure independent enhancement pattern. Short-axis cine images were analyzed for assessment of left ventricular (LV) volumes, ejection fractions (EF), first-perfusion images for slope, max signal intensity, time to peak, time to 50% max with dedicated software (Cmr42,Circle Cardiovascular Imaging Inc.,Calgary, Canada). The correlation between methods was evaluated with two-variable linear regression analysis, with Pearson correlation.Results
All rabbits survived after MRI scanning without significant differences in heart rate, LV end-diastolic volume, end-systolic volume and EF between baseline and after injection of Gd or Mn (p>0.05). First-pass perfusion MRI identified infarcted myocardial segments when compared with normal myocardial segments. When compared with normal myocardial segments, the slope, max signal intensity of infarcted myocardial segments decreased significantly, time to peak and time to 50% max extended (all p<0.05). All the perfusion parameters of infarcted and normal myocardial segments correlated well between Gd-based and Mn-based perfusion imaging (all p<0.05, r=0.53-0.86).Conclusion
Our novel Mn2+ Chelate contrast agent is safe and reliable to visualize myocardial perfusion in myocardial infarction.Acknowledgements
This work was supported by the National Natural Science Foundation of China (81471721, 81471722, 81641169, 81771887 and 81771897), Program for New Century Excellent Talents in University (no: NCET-13-0386), and Program for Young Scholars and Innovative Research Team in Sichuan Province (2017TD0005) of China.References
1. Hundley WG, Bluemke DA, Finn JP, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 exert consensus document on cardiaovascular magnetic resonance. J Am Coll Cardiol 2010; 55(23): 2614-62
2. System USRD. 2014 USRDS annual data report: An overview of the epidemiology of kidney disease in the United States. 2014.
3. Fox CS, Muntner P, Chen AY, Alexander KP, Roe MT, Cannon CP, et al. Use of Evidence-Based Therapies in Short-Term Outcomes of ST-Segment Elevation Myocardial Infarction and Non–ST-Segment Elevation Myocardial Infarction in Patients With Chronic Kidney Disease A Report From the National Cardiovascular Data Acute Coronary Treatment and Intervention Outcomes Network Registry. Circulation. 2010; 121(3): 357-65.
4. Su H, Wu C, Zhu J, Miao T, Wang D, Xia C, et al. Rigid Mn (II) chelate as efficient MRI contrast agent for vascular imaging. Dalton Transactions. 2012; 41(48): 14480-3.
Figures
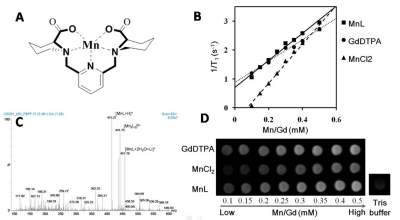
Fig 1. Representations (A) and Mass spectrometry (C) of the molecular structure of the chelate [Mn3L2(H2O)4Cl2]; B. T1 relaxation rate (1/T1, s-1) as a function of Mn2+ or Gd3+ concentration (mM) at 20 ℃, 1.5 T; D. T1-weighted MRI images of Gd-DTPA, MnCl2 and Mn chelate.