3477
Infarct Pattern and Large Artery Atherosclerosis Features Revealed by Combined Intra- and Extra-cranial Vessel Wall Imaging in Patients with Non-cardiac Acute and Sub-acute Ischemic StrokeNa Zhang1, Jinhao Lyu2, Lei Zhang1, Lin Jia3, Wenxiao Jia3, Hairong Zheng1, and Xin Liu1
1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, 2Department of Radiology, Chinese PLA General Hospital, Beijing, China, 3XinJiang Medical University, Urumchi, China
Synopsis
Infarct pattern referring single or multiple infarction lesions of patients with ischemic stroke is a feasible imaging marker to predict future stroke recurrence. The aim of this study was to detect large artery atherosclerosis features resulting in single or multiple infarction lesions in patients with non-cardiac acute and sub-acute ischemic stroke using the combined intra- and extra-cranial vessel wall MR imaging method. The results demonstrated that in large artery atherosclerosis, infarct pattern may be associated with the vulnerability of atherosclerotic plaques, and this combined imaging method can be used to explore the vascular pathology and predict recurrence of ischemic stroke.
Introduction
Infarct pattern referring single or multiple infarction lesions of patients with ischemic stroke is a feasible imaging marker to predict future stroke recurrence [1]. The underlying mechanism of infarct pattern due to large artery atherosclerosis has not been well studied. Taking advantage of the newly developed three dimensional (3D) combined intra- and extra-cranial vessel wall magnetic resonance (MR) imaging technique based on T1 weighted variable-flip-angle turbo spin echo (SPACE) with isotropic 0.55 mm high resolution and improved cerebrospinal fluid suppression [2], it is capable to visualize the arterial vessel wall from common carotid artery to distal segments of intracranial arteries for comprehensive evaluating ischemic stroke etiology and recurrence risk. The aim of this study was to detect large artery atherosclerosis features resulting in single or multiple infarction lesions in patients with non-cardiac acute and sub-acute ischemic stroke using the combined intra- and extra-cranial vessel wall MR imaging method.Materials and Methods
The study was approved by the local institutional review board and all patients had given the written informed consent before MR imaging. 55 patients with non-cardiac acute and subacute ischemic stroke were retrospectively collected from 2016 to 2017 in one imaging center. Inclusion criteria included ischemic stroke confirmed by diffusion weighted imaging (DWI) within 30 days and caused by larger artery disease. Patients with potential cardiac embolism were excluded. All patients had underwent routine MR Imaging, DWI and 3D high resolution combined intra- and extra-cranial vessel wall MR imaging with (post-contrast) and without contrast agent (Figure 1) on a 3T MR system (MAGNETOM TIM Trio, Siemens, Germany). Stroke etiology was diagnosed according to both imaging findings and clinical evidences by two experienced neurologists in consensus. Based on DWI findings, patients were divided into 2 groups for comparison according to infarct pattern: (1) single infarction lesion in one vascular territory, and (2) multiple infarction lesions in single or multiple vascular territories. For patients with large artery atherosclerosis, the location and number of the plaques identified with focal or diffuse eccentric vessel wall thickening were recorded. In addition, all detected plaques were then categorized based on plaque location (Intracranial or extracranial arterial plaques) and infarct pattern (single-lesion or multiple-lesion pattern). Also the culprit and non-culprit plaques were discriminated by the same two neurologists with consensus according to Qiao et al [3]. For post-contrast vessel wall images, plaque enhancement was assessed as Grade 0 (no enhancement or similar to the enhancement of normal vessel wall), Grade 1 (mild to moderate enhancement less than post-contrast pituitary), and grade 2 (obvious enhancement similar to post-contrast pituitary). Intraplaque hemorrhage was also identified. The clinical demographics of the patients with large artery atherosclerosis and characteristics of the identified culprit plaques were statistically compared between single-lesion and multiple-lesion groups. A comparison for characteristics of all detected plaques between intracranial and extracranial arteries was also performed.Results
A total of 55 patients (45.53±12.06 years, 46 male) were included in the study. 19 patients showed single-lesion pattern and 36 patients showed multiple-lesion pattern. The stroke etiology was diagnosed as follows: large artery atherosclerosis: 43; artery dissection: 3; Moyamoya disease: 2; vasculitis: 2 and other etiology: 5. There was no significant difference of the stroke etiology between single-lesion group and multiple-lesion group. Among the 43 patients with large artery atherosclerosis, 14 patients showed single-lesion pattern and 29 patients showed multiple-lesion pattern. And 21 and 64 culprit lesions were identified in the two groups, respectively. The clinical demographics of the 43 patients and characteristics of the identified culprit plaques for the two patterns were summarized in Table 1. Plaque enhancement of culprit plaques was significantly more prominent in multiple-lesion pattern group than single-lesion pattern group (p=0.004). A representative single-lesion pattern diagnosed on DWI image and the culprit plaque identified on vessel wall MR images were shown in Figure 2. The comparison of all detected plaques of patients with large artery atherosclerosis between intracranial and extracranial arteries were summarized in Table 2. There was significant difference of prevalence of culprit lesion between intracranial and extracranial arteries (p=0.009).Discussion and Conclusion
The results of this study indicate that in large artery atherosclerosis, infarct pattern may be associated with the vulnerability of atherosclerotic plaques. And compared with intracranial arterial plaques, extracranial arterial plaques may characterize more vulnerability. And this is still needed to be confirmed in a large-scale patients with arterial atherosclerosis in our near future study. In conclusion, the 3D combined vessel wall imaging is a clinical useful approach and can be used to explore the vascular pathology and predict recurrence of ischemic stroke.Acknowledgements
This work was supported in part by National Key R&D Program of China (2016YFC0100100) and Key Laboratory for Magnetic Resonance and Multimodality Imaging of Guangdong Province (2014B030301013).References
1. Wen H et al. Neurology, 2004;63(7): 1317-1319. 2. Zhang L et al. MRI 2017; 44:65-71. 3. Qiao Y et al. Radiology 2014; 271(2): 534-542.Figures
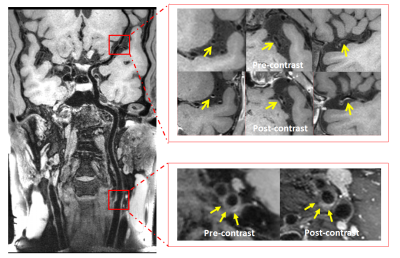
Figure 1 Representative 3D vessel wall MR images acquired
using the high resolution combined intra- and extra-cranial arterial vessel
wall imaging technique for a 44-year-old male patient. The image shows large
spatial coverage from common carotid artery (CCA) to distal segment of whole
brain intracranial arteries and satisfactory image quality. Two eccentric
atherosclerotic plaques (arrows) were detected in internal carotid artery (ICA)
and middle cerebral artery (MCA) with moderate enhancement on post-contrast
vessel wall images, respectively.
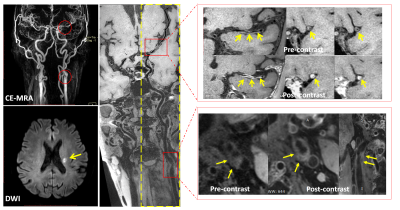
Figure 2 Representative MR images of a 60-year-old male
patient with single-lesion infarct pattern. The large eccentric atherosclerotic
plaque (arrows) with prominent enhancement affected M1 segments of left middle
cerebral artery is considered as the culprit lesion. And the other plaque (arrows)
located in the carotid artery bifurcation with moderate enhancement is
considered as the non-culprit lesion. The corresponding arterial stenosis are
observed on CE-MRA images. CE-MRA: contrast enhanced MR angiography. DWI:
diffusion weighted imaging.

Table 1 Clinical demographics of the patients with large
artery atherosclerosis and characteristics of the identified culprit plaques
for different lesion patterns.
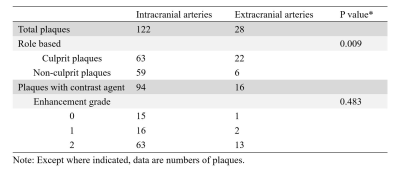
Table 2 Characteristics of all detected plaques in
intracranial and extracranial arteries of patients with large artery
atherosclerosis.