3359
Truncation Artifact in Pulmonary Magnetic Resonance Angiography1Radiology, University of Wisconsin - Madison, Madison, WI, United States, 2Medical Physics, University of Wisconsin - Madison, Madison, WI, United States, 3Medicine, University of Wisconsin - Madison, Madison, WI, United States, 4Biomedical Engineering, University of Wisconsin - Madison, Madison, WI, United States, 5Emergency Medicine, University of Wisconsin - Madison, Madison, WI, United States
Synopsis
Pulmonary magnetic resonance angiography is a promising technique for the detection of pulmonary embolism but suffers from central vessel dropout (truncation artifact) that can mimics emboli in medium-sized vessels. Corner-cutting k-space acquisition strategies are suspected to exacerbate this artifact. Simulations and in vivo experiments were used to investigate the relationship between corner-cutting and truncation artifact. Our simulations suggest that eliminating corner-cutting reduces the symmetry and magnitude of the ringing with this artifact but we observed only minor differences in volunteers. We conclude that corner-cutting, which can be used to shorten scan times and/or improve spatial resolution, does not exacerbate the central vessel dropout artifact.
Introduction
Pulmonary magnetic resonance angiography (MRA) is a promising non-ionizing alternative for the detection of pulmonary embolism(PE)1,2. However, pulmonary MRA can suffer from central vessel dropout3,4 (often termed “truncation artifact”) that mimics PE and could decrease diagnostic accuracy, particularly with radiologists inexperienced with pulmonary MRA.
Corner-cutting is a well-known strategy with 3D MRI methods, such as MRA, to reduce scan time and/or improve spatial resolution with only a small reduction in SNR and resolution in the diagonal direction5. Corner-cutting k-space sampling is a useful approach to obtain high-resolution images that cover the lungs in a short breath-hold (<20s) with good signal to noise ratio (SNR) performance.
However, corner-cutting k-space sampling is suspected to cause or exacerbate the pulmonary embolus mimicking central vessel dropout artifact. The purpose of this study was to investigate the relationship between corner-cutting and the truncation artifact in pulmonary MRA to determine whether the central vessel dropout artifact can be mitigated by removing corner-cutting.
Methods
Simulations were used to predict the differences between undersampling schemes with and without corner-cutting. Simulated results were then compared to ferumoxytol-enhanced pulmonary MRA in volunteers.
Simulations
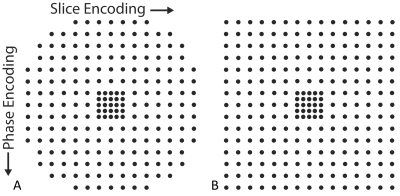
Simulations of a solid cylinder (radius of 7 pixels) were performed with conventional undersampling schemes with corner-cutting, where 78% of k-space was sampled in a circularly symmetric pattern (Figure 1a), and without corner-cutting (Figure 1b). Image reconstructions were performed using the Autocalibrating Reconstruction for Cartesian imaging (ARC) reconstruction6. The reconstructed images had a nominal acceleration factor of two in both phase and slice encoding, outside the calibration region.
MRI Measurements
Fourteen healthy volunteers were recruited and scanned on a 3T clinical MRI system (Discovery MR750, GE Healthcare, Waukesha, WI) using a 32-channel torso coil (NeoCoil, Pewaukee, WI). Specifically, a 4mg/kg dose of ferumoxytol (Feraheme, AMAG Pharmaceuticals, Waltham, MA) was diluted up to 30 mL and injected according to recently published guidelines on the safe administration of ferumoxytol for MRI7. Imaging was performed approximately 10 minutes after the injection was completed to ensure that the ferumoxytol was in steady state. We note that ferumoxytol has a half-life of approximately 14-15 hours, so all imaging was performed in an intravascular steady state and was thus easier to compare between two acquisitions acquired minutes apart.
Undersampled 3D-spoiled gradient echo (SGRE) acquisitions with a sagittal-excitation/coronal reconstruction strategy8 were performed using sampling schemes with and without corner-cutting. Both scans had a resolution of 1.9x1.8x1.5mm (LRxAPxSI), 1.0ms TE, and a nominal acceleration factor of two in both phase and slice encoding directions. Only the TR and receiver bandwidth (rBW) changed between the two scans to achieve a constant 19s scan time in both, which is an acceptable breath-hold for most volunteers. The corner-cutting scan had BW=±83kHz rBW and TR=2.8ms, while the no corner-cutting scan had BW=±125kHz and TR=2.4ms.
Results
Simulations
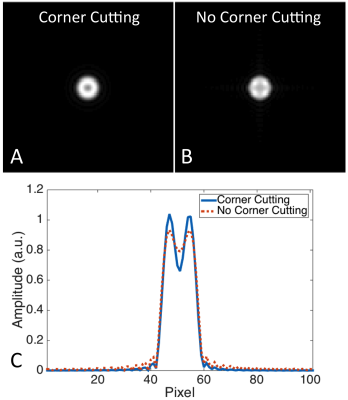
Simulated results of sampling a solid cylinder are shown in Figure 2 using both corner-cutting and no corner-cutting. Eliminating corner-cutting reduces the symmetry of the central darkening in Figure 2A and 2B as well as decreases the magnitude of the ringing in the cylinder as shown in the horizontal profile in Figure 2C.
MRI Measurements
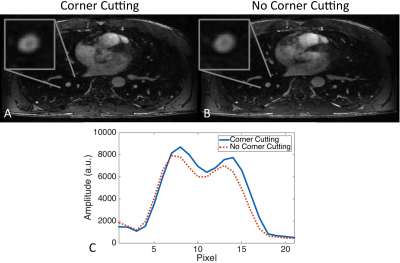
Example reconstructions from a volunteer are shown in Figure 3. The symmetry and the magnitude of the ringing inside the vessel do not seem to be affected by the inclusion of corner-cutting. Similar results were seen in all the other patients.
Discussion & Conclusions
This study investigated the relationship between corner-cutting and the truncation artifact in pulmonary MRA using both simulations and in vivo contrast enhanced MRA studies. Our simulations suggested that eliminating corner-cutting should reduce the symmetry and magnitude of the ringing causing the central vessel darkening. However, these predictions were not observed in volunteers, where no significant differences between the two acquisitions were observed. These results suggest that utilizing corner-cutting allows shorter scan times, higher resolution images, with good signal to noise properties and does not exacerbate the central vessel dropout artifact. Further investigation is still needed to determine what other factors contribute to this artifact and where it can be eliminated or mitigated.Acknowledgements
The Departments of Radiology and Medical Physics, University of Wisconsin supported this project. The authors also wish to acknowledge support from GE Healthcare, the National Cancer Institute of the National Institutes of Health under Award Number T32CA009206, and the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number K24 DK102595.References
1. Schiebler ML, Nagle SK, Francois CJ, Repplinger MD, Hamedani AG, Vigen KK, Yarlagadda R, Grist TM, Reeder SB. Effectiveness of MR angiography for the primary diagnosis of acute pulmonary embolism: clinical outcomes at 3 months and 1 year. J Magn Reson Imaging. 2013;38(4):914-25.
2. Kalb B, Sharma P, Tigges S, Ray GL, Kitajima HD, Costello JR, Chen Z, Martin DR. MR imaging of pulmonary embolism: diagnostic accuracy of contrast-enhanced 3D MR pulmonary angiography, contrast-enhanced low-flip angle 3D GRE, and nonenhanced free-induction FISP sequences.
3. Bannas P, Schiebler ML, Motosugi U, Francois CJ, Reeder SB, Nagle SK. Pulmonary MRA: differentiation of pulmonary embolism from truncation artefact. Eur Radiol. 2014;24(8):1942-9.
4. Nagle SK, Schiebler ML, Repplinger MD, Francois CJ, Vigen KK, Yarlagadda R, Grist TM, Reeder SB. Contrast enhanced pulmonary magnetic resonance angiography for pulmonary embolism: Building a successful program. Eur J Radiol. 2016;85(3):553-63.
5. Bernstein MA, Fain SB, Riederer SJ. Effect of windowing and zero-filled reconstruction of MRI data on spatial resolution and acquisition strategy. J Magn Reson Imaging. 2001;14(3):270-80.
6. Beatty P, Brau A, Chang S, Joshi S, Michelich C, Bayram E, Nelson T, Herfkens R, Brittain J, A Method for Autocalibrating 2-D Accelerated Volumetric Parallel Imaging with Clinically Practical Reconstruction Times, In Proceedings of the 15th Annual Meeting of ISMRM, Berlin, Germany, 2007. Page 1749.
7. Safety and technique of ferumoxytol administration for MRI. Vasanawala SS, Nguyen KL, Hope MD, Bridges MD, Hope TA, Reeder SB, Bashir MR. Magn Reson Med. 2016 May;75(5):2107-11. doi: 10.1002/mrm.26151. Epub 2016 Feb 18. Review.
8. Brau A, Bayram E, Saranathan M, Kawashima A, Rotated Slab Excitation (ROSE) for Reduced Foldover Artifacts in Coronal 3D Abdominal Imaging, In Proceedings of the 16th Annual Meeting of ISMRM, Toronto, Canada, 2008. Page 502.
Figures