3348
Application of non-contrast-enhanced MR angiography in hepatic arteriography1Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Synopsis
Accurate evaluation of hepatic arterial anatomy and variants is essential for preoperative planning of hepatic resection, transarterial chemoembolization and liver transplantation. In the present study, we try to explore the value of non-contrast-enhanced MR angiography using spatial labeling with multiple inversion pulses (SLEEK-MRA) in hepatic arteriography, and to compare the results with CT angiography (CTA). Although SLEEK-MRA was inferior to CTA in depicting small branches, it was comparable to CTA for depiction of the common hepatic artery, proper hepatic artery, left hepatic artery and right hepatic artery. As a noninvasive angiography method, SLEEK-MRA is valuable in hepatic arteriography.
Introduction
Accurate evaluation of hepatic arterial anatomy and variants is essential for preoperative planning of hepatic resection, transarterial chemoembolization and liver transplantation. Digital subtraction angiography is the criterion standard for hepatic vascularity, but the radiation, contrast medium, and complications associated with catheterization should be considered. Contrast-enhanced CT angiography is an non-invasive procedure for the detailed evaluation of the hepatic arterial anatomy. However, the need for iodinated contrast medium and ionizing radiation are disadvantages. Recently, non-contrast-enhanced MR angiography using spatial labeling with multiple inversion pulses (SLEEK-MRA) have made rapid progress and is effectively used for visualization of the renal artery and renal vein.1-3 The purpose of this study was to explore the value of SLEEK-MRA in hepatic arteriography, and to compare the results with CT angiography (CTA).Methods
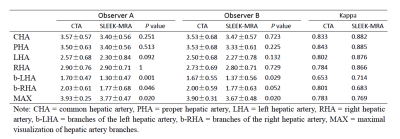
Patients (n=37) who had undergo both CTA and SLEEK-MRA examinations were enrolled in this study. SLEEK-MRA were performed within 7 days after finished with CTA. Images of CTA and SLEEK-MRA were analyzed by two abdominal radiologists to evaluate the image quality (four-point scale) and the ability of maximal visualization of hepatic artery branches (the codes were:1 for the common hepatic artery; 2 for the proper hepatic artery; 3 for the left/right branch of the hepatic artery; and 4 for branches of the left or right hepatic artery). Differences between CTA and SLEEK-MRA in image quality and the ability of maximal visualization of hepatic artery branches were compared with the Wilcoxon signed-rank test.Results
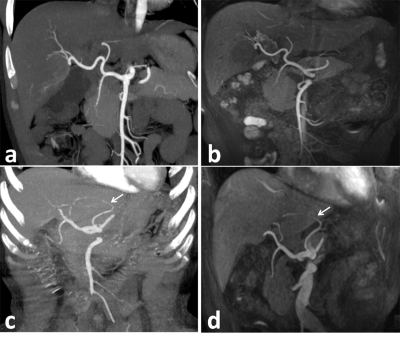
The interobserver agreement between two radiologists was good to excellent (Kappa: CTA, 0.653-0.843; SLEEK-MRA, 0.683-0.885). Except for the first branches of the left and right hepatic artery, CTA and SLEEK-MRA showed no statistical differences in image quality in the common hepatic artery, proper hepatic artery, left hepatic artery and right hepatic artery (all P>0.05). CTA was superior to SLEEK-MRA in displaying the largest artery branches (P=0.020). Among 37 patients, there were 7 patients whose hepatic arteries were variant and SLEEK-MRA visualized 6 of these cases.Discussion
In present study, SLEEK-MRA was used to evaluate the hepatic arterial anatomy and variants without using contrast medium. The preliminary data demonstrate that, except the branches of the left and right hepatic artery, SLEEK-MRA was comparable to CTA for depiction of the common hepatic artery, proper hepatic artery, left hepatic artery and right hepatic artery. SLEEK-MRA has the advantage of avoiding certain interfering factors, such as spinal bones, atherosclerotic plaques, and the early venous system enhancement, in comparison with CTA. However, SLEEK-MRA was inferior to CTA in depicting small branches. The reason may be related to the following factors: first, the blood flow in small branches is small, causing weak signal intensity in SLEEK-MRA; and second, the small branches are far away from the abdominal aorta, which indicated that it would take a relatively long time for the in-flow blood to arrive at the small branches in comparison with the blood suppression inversion time (BSP TI). To some extent, a long BSP TI is suitable for small branches delineation, but extended BSP TI values deteriorate vessel-to-liver contrast because of signal recovery in the surrounding tissue. Therefore, BSP TI selection needs to strike a balance between vessel-to-liver contrast and artery visualization.Conclusion
As a noninvasive angiography method, SLEEK-MRA avoids radiation and the use of contrast agent, it is valuable in hepatic arteriography.Acknowledgements
No acknowledgement found.References
1. Tang H, Wang Z, Wang L, et al. Depiction of transplant renal vascular anatomy and complications: unenhanced MR angiography by using spatial labeling with multiple inversion pulses. Radiology. 2014; 271(3):879-887.
2. Pei Y, Shen H, Li J, et al. Evaluation of renal artery in hypertensive patients by unenhanced MR angiography using spatial labeling with multiple inversion pulses sequence and by CT angiography. AJR Am J Roentgenol. 2012; 199(5):1142-1148.
3. Pei Y, Li F, Shen H, et al. Optimal Blood Suppression Inversion Time Based on Breathing Rates and Heart Rates to Improve Renal Artery Visibility in Spatial Labeling with Multiple Inversion Pulses: A Preliminary Study. Korean J Radiol. 2016; 17(1):69-78.
Figures