3343
MR time optimization: 2-year institutional experience in clinically applied high-resolution intracranial vessel wall imaging1Department of Radiology & Biomedical Imaging, University of California, San Francisco, San Francisco, CA, United States
Synopsis
High-resolution intracranial vessel wall imaging (VWI) can provide valuable information not only regarding vascular morphology but also about the presence or absence of vessel wall enhancement; however, VWI acquisition times are often long, limiting routine use in clinical practice. We sought to investigate the use of the VWI in routine clinical practice to evaluate its application within our institution as well as optimize the imaging protocol to meet clinical needs. Our study found post-contrast VWI better demonstrated the vascular pathology compared to pre-contrast VWI. We also found only one case that may have benefited from the addition of pre-contrast VWI; however, the addition of pre-contrast VWI in this case would not have changed clinical management. Our findings suggest that the routine use pre-contrast VWI may not be needed to obtain the imaging necessary for clinical diagnosis and patient management.
Introduction
High-resolution intracranial vessel wall imaging (VWI) can provide valuable information not only regarding vascular morphology1 but also about the presence or absence of vessel wall enhancement;2-4 however, VWI acquisition times are often long, limiting routine use in clinical practice. We sought to investigate the use of the VWI in routine clinical practice to evaluate its application within our institution as well as optimize the imaging protocol to meet clinical needs.Methods
A search was conducted of all studies obtained for routine clinical practice using the UCSF high-resolution intracranial vessel wall imaging protocol from 10/20/2015 through 10/19/2017. MRIs obtained for research purposes were excluded. The UCSF VWI protocol includes both pre- and post-contrast high-resolution 3D CUBE T1-weighted intracranial vessel wall images. The clinical VWI GE protocol is as follows: 0.6mm slice thickness, 240 slices, 16cm FOV and 320x320 FOV, 0.5mm in-plane resolution; echo train length 60; TR/TE 1000ms/10ms; GRAPPA 2 acceleration, scan time 9 minutes. Qualitative image quality was assessed for both pre- and post-contrast imaging using a four-point scale: 0 = non-diagnostic; 1 = vessel wall seen in part, diagnostic quality; 2 = vessel wall seen clearly in most parts, good image quality; and 3 = sharp vessel wall confidently delineated; excellent image quality. The images were also evaluated for the presence of vessel wall enhancement, detection of the vascular pathology on pre-contrast VWI alone, and detection of the vascular pathology on post-contrast VWI alone (dichotomized as either YES or NO).Results
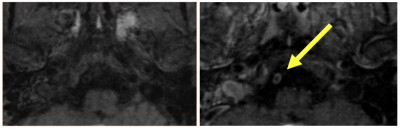
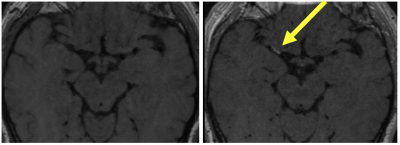
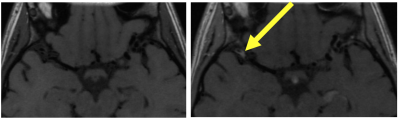
During this 2-year period, 82 MRI examinations using the VWI protocol were obtained. Five patients had multiple examinations with 4 subjects having 2 scans and 1 subject having 5 scans. Eight of the examinations had no vascular pathology. There was no statistically significant quality difference between the pre- (2.75 ± 0.51) and post-contrast (2.78±0.52) VWI scans (p=0.53; paired t-test). Pre-contrast VWI detected the pathology in 62/74 MR examinations with disease. Post-contrast VWI detected the pathology in 71/74 examinations with only 3 cases not showing the pathology on the post-contrast scan (p=0.002). 81/82 of the scans did not benefit from the addition of pre-contrast imaging with one case of vertebral artery dissection showing intrinsic T1 hyperintensity on pre-contrast.Discussion
Our study found post-contrast VWI more often demonstrated the vascular pathology compared to pre-contrast VWI. We also found only one case that might have benefited from the addition of pre-contrast VWI; however, the addition of pre-contrast VWI would not have changed clinical management. This suggests that the routine use of pre-contrast VWI may not be needed to obtain the imaging necessary for routine clinical diagnosis and patient management.Conclusion
Routine use of pre-contrast VWI imaging may be unnecessary. Obtaining only post-contrast VWI would reduce acquisition times, potentially making VWI more accessible in the clinical setting.Acknowledgements
References
1. Li ML, Xu YY, Hou B, et al. High-resolution intracranial vessel wall imaging using 3D CUBE T1 weighted sequence. Eur J Radiol. 2016 Apr;85(4):803-7. doi: 10.1016/j.ejrad.2016.01.014. Epub 2016 Jan 21.
2. Mandell DM, Mossa-Basha M, Qiao Y, Hess CP, et al; Vessel Wall Imaging Study Group of the American Society of Neuroradiology. Intracranial Vessel Wall MRI: Principles and Expert Consensus Recommendations of the American Society of Neuroradiology.AJNR Am J Neuroradiol. 2017 Feb;38(2):218-229. doi: 10.3174/ajnr.A4893. Epub 2016 Jul 28.
3. Mossa-Basha M, Shibata DK, et al. Added Value of Vessel Wall Magnetic Resonance Imaging for Differentiation of Nonocclusive Intracranial Vasculopathies. Stroke. 2017 Nov;48(11):3026-3033. doi: 10.1161/STROKEAHA.117.018227. Epub 2017 Oct 13.3.
4. de Havenon A, Mossa-Basha M, Shah L, et al. High-resolution vessel wall MRI for the evaluation of intracranial atherosclerotic disease. Neuroradiology. 2017 Sep 23. doi: 10.1007/s00234-017-1925-9.
Figures