3342
Feasibility and Optimization of Ultra-Short Echo Time MRI for Improved Imaging of IVC Filters1Department of Radiology, University of Wisconsin – School of Medicine and Public Health, Madison, WI, United States, 2Department of Medical Physics, University of Wisconsin – School of Medicine and Public Health, Madison, WI, United States, 3Department of Pediatrics, University of Wisconsin – School of Medicine and Public Health, Madison, WI, United States, 4Department of Biomedical Engineering, University of Wisconsin – School of Medicine and Public Health, Madison, WI, United States, 5Department of Medicine, University of Wisconsin – School of Medicine and Public Health, Madison, WI, United States, 6Department of Emergency Medicine, University of Wisconsin – School of Medicine and Public Health, Madison, WI, United States
Synopsis
Monitoring of inferior vena cava (IVC) filters for complications is commonly performed using CTA. It would be desirable to evaluate IVC-filters using MRA to avoid the need for ionizing radiation and to exploit the superior soft tissue contrast of MRA. Unfortunately, conventional contrast enhanced MRA (cMRA) techniques are limited by distortion and signal voids arising from metal in the IVC-filter. In this pilot study, we evaluated the feasibility of ultra-short echo time (UTE) MRA at 3.0T in nine patients with IVC-filters. Results demonstrate feasibility of free-breathing UTE-MRA for the assessment of IVC-filters with comparable IVC-depiction compared to cMRA.
Introduction
Inferior vena cava (IVC) filters are used to prevent the passage of deep-vein thrombi (DVT) to the pulmonary arteries in patients with acute proximal deep-vein thrombosis or pulmonary embolism and absolute contraindications to anticoagulation [1]. IVC-filters are prone to complications including IVC-perforation, filter migration, thrombotic occlusion or fracture, among others [1; 2]. CTA is commonly used to assess IVC-filters for complications. Unfortunately, CTA requires ionizing radiation, and DVT is common in young patients. MRA has been limited for the evaluation of IVC-filters due to distortion and signal voids resulting from metal in the filter [2]. We sought to determine the feasibility and optimize the imaging protocol of ultra-short echo time (UTE) MRA for the assessment of IVC-filters.
Methods
Patients with implanted IVC-filters, who were identified from either CTA or conventional venography, were recruited for this prospective IRB-approved, HIPAA-compliant feasibility study. Written informed consent was obtained. Patients with contraindications to contrast-enhanced MRA were excluded.
Imaging was performed on a 3.0T MRI-system (MR750, GE Healthcare, Waukesha, WI) using a 32-channel phased-array torso coil (Neocoil, Pewaukee, WI). After intravenous injection of 0.05mmol/kg gadofosveset trisodium (Ablavar®, Lantheus, Billerica, MA), all patients underwent conventional multi-phase breath-held MRA (cMRA), followed by two radial-acquisition UTE-techniques: breath-held UTE-MRA (bhUTE) and free-breathing UTE-MRA (fbUTE). Both UTE-methods were acquired at three flip angles (10°,15°,20°) to optimize T1-weighting for best depiction of the IVC and IVC-filter (sequence parameters: Table 1).
Two radiologists independently assessed image quality (IQ) of bhUTE-(15°), fbUTE-(15°) and venous-phase cMRA (Table 2).
A questionnaire was also used to ascertain the reasons for impaired IVC-filter depiction and whether artifacts reduced reader confidence to assess IVC-filter related complications (Table 3).
To determine the optimal flip angle (FA) regarding “Quality of IVC-Filter Depiction” and “Quality of the IVC-Venogram”, an IQ-ranking across UTE-FA was performed in a separate consensus reading.
One reader determined the relative signal-intensity (SIrel) ratios between the filter-cavity and the IVC caudal of the filter to assess signal voids within the filter-cavity.
Statistics: Friedman- and Wilcoxon-Signed-Ranks-test were used to assess IQ-differences and FA-rankings. Data from IQ-readings are presented as absolute and relative frequencies with medians and interquartile ranges (IQR). Categorical data from the questionnaire are presented as relative frequencies across readers.
Inter-rater reliability were assessed using the intraclass correlation coefficient (ICC) for average measures and Spearman-Rank correlation (r2).
SIrel-ratios (filter-cavity/IVC) between the methods were compared with a paired sample t-test. Two-sided p-values <0.05 were regarded as statistically significant. Calculations were performed using SPSS (IPSS Inc., version 23.0, IBM, Chicago, IL).
Results
Nine patients were included (7:2 M:F; 57.6±11.7 years; 87.4±7kg).
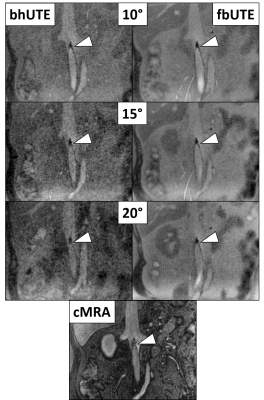
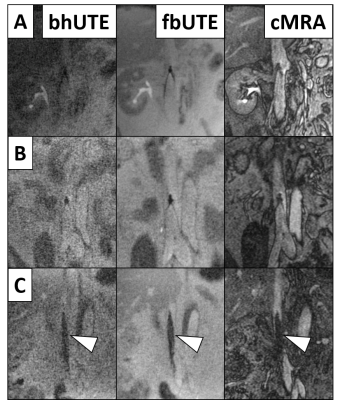
Representative image examples of bhUTE, fbUTE and cMRA are shown in Figures 1 and 2. Table 2 summarizes the IQ-ratings across readers. Table 3 summarizes the reasons for impaired IQ-ratings.
IQ-Differences:
IVC-filter depiction: No significant difference regarding the quality of IVC-filter depiction was detected between fbUTE-(15°) and cMRA. bhUTE-(15°) showed the lowest IQ for the IVC-filter depiction.
Presence of artifacts: No significant difference regarding image artifacts was observed between fbUTE-(15°) and cMRA. bhUTE-(15°) showed significantly more artifacts than fbUTE and cMRA (p<0.05 across readers).
IVC-venogram: The subjective quality of the IVC-venogram was rated significantly better with cMRA compared to both UTE-techniques (p<0.05), due to better contrast between the IVC and surrounding tissue using cMRA.
Differences between UTE-FA:
With bhUTE, a FA of 10° rated best in terms of the quality of IVC-filter depiction (p<0.05), whereas FAs of 10° and 15° were equal with respect to the quality of the IVC-venogram.
For fbUTE, a FA of 10° was rated best for both, quality of IVC-filter depiction and quality of IVC-venogram (p<0.05).
Inter-reader reliability was moderate (ICC=0.77 [CI: 0.64; 0.85],r2=0.62).
SIrel-ratios:
No significant differences in SIrel-ratios (filter-cavity/IVC) were observed between the three methods. All three techniques showed a slightly lower SIrel within the filter-cavity compared to the IVC: cMRA=0.9±0.2, bhUTE=0.9±0.2, fbUTE=0.8±0.2.
Discussion
In this study, we found that free-breathing radial-acquisition UTE-MRA shows comparable IQ to conventional Cartesian-MRA, with best results at a flip angle of 10°.
The quality of the IVC-venogram was rated superior using cMRA in the subjective IQ-readings due to a better contrast between the IVC and surrounding tissue. Breath-held UTE-MRA had overall inferior IQ and higher rates of artifacts.
All three MRA-techniques showed only minor signal voids within the filter-cavity.
Conclusion
UTE-MRA may be feasible for the assessment of IVC-filters, particularly using a free-breathing protocol. The ultra-short echo times, combined with radial sampling could help to mitigate metal- and motion-related artifacts, respectively. Larger studies should investigate the clinical utility of free-breathing UTE-MRA for assessment of IVC-filter related complications.
Acknowledgements
This project was supported by the Departments of Radiology and Medical Physics, at the University of Wisconsin. The authors also wish to acknowledge support from GE Healthcare and Bracco Diagnostics who provide research support to the University of Wisconsin. Further, we also wish to acknowledge support from the NIH (K24 DK102595).
Tilman Schubert contributed to this work while employed by UW-Madison but is now an employee of the Department of Radiology, University Hospital Bern, Switzerland.
Peter Bannas contributed to this work while employed by UW-Madison but is now an employee of the Department of Radiology and Nuclear Medicine, University Hospital Hamburg-Eppendorf, Germany.
Nathan Artz contributed to this work while employed by UW-Madison but is now an employee of the Department of Diagnostic Imaging, St. Jude Children's Research Hospital, Memphis, TN.
References
1 Duffett L, Carrier M (2017) Inferior vena cava filters. J Thromb Haemost 15:3-12
2 Sildiroglu O, Ozer H, Turba UC (2012) Management of the thrombosed filter-bearing inferior vena cava. Semin Intervent Radiol 29:57-63
Figures
Acquisition parameters for conventional MRA, breath-held UTE and free-breathing UTE at 3.0T.
Results of image quality ratings across readers:
The quality of IVC-filter depiction was comparable between free-breathing UTE (fbUTE) and conventional MRA (cMRA). The quality of the IVC-filter depiction with breath-held UTE (bhUTE) was significantly lower than both, fbUTE and cMRA, p<0.05.
The rate of artifacts between fbMRA and cMRA did not differ significantly. bhUTE had overall higher rates of poor image quality and significantly more artifacts than fbUTE (p<0.001) and cMRA (p<0.05).
The quality of the IVC-venogram was significantly better with cMRA compared to bhUTE (p<0.001) and fbUTE (p<0.05).