3339
Three-dimensional MRA Demonstrates Eccentric Enlargement of the Non-Conjoined Cusp-Sinus in Bicuspid Aortic Valve Patients1Northwestern University, chicago, IL, United States, 2Department of Cardiovascular Medicine, Mayo Clinic, Rochester, Rochester, MN, United States, 3AMNCH Tallaght Hospital, Dublin, Ireland
Synopsis
Bicuspid aortic valve is associated with ascending aortic dilatation, including the aortic root. The etiology of this aortopathy is controversial, with contributions proposed to come from both genetic and hemodynamic origins. While the pattern of aortic dilatation has been loosely associated with cusp fusion patterns and valve function, no study has investigated if eccentric sinus dilation is present and whether it varies in relation to the BAV phenotype. Thus, this study uses b-SSFP cine imaging and gated CE-MRA or 3D IR SSFP to assess the structure of the bicuspid aortic valve and identify the presence of a dominant sinus.
Introduction
Patients with bicuspid aortic valve (BAV) often develop aortopathy with dilatation of one or more thoracic aorta segments, which may include the aortic root (Sinus of Valsalva), ascending aorta or aortic arch. Thoracic aorta dilatation is a risk factor for complications such as dissection. In addition, a “root phenotype” with predominating sinuses of Valsalva dilatation have been described, which could carry higher dissection risk (1). There is active debate whether BAV aortopathy results from an inherited predisposition or from abnormal transvalvular flow, with evidence supporting both theories (1). Insights into these mechanisms may ultimately impact surveillance and management guidelines in these patients. To investigate these hypotheses, studies have focused on absolute maximal dimensions of aortic segments, and less on their symmetry. Assessment of the symmetry of the aortic root could shed light into the mechanisms of BAV aortopathy. Although segmental thoracic aorta dilatation has been found to be associated with specific BAV cusp fusion patterns and valve function (2, 3); little is known about the symmetry of the BAV root and the presence of eccentric root dilation and its association with cusp fusion patterns. Thus, this study assesses the associations between BAV phenotypes and root symmetry.Methods
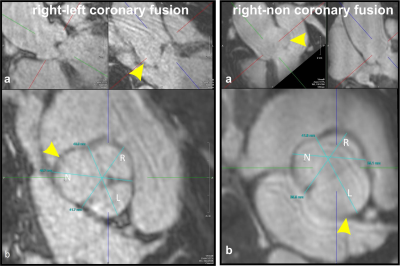
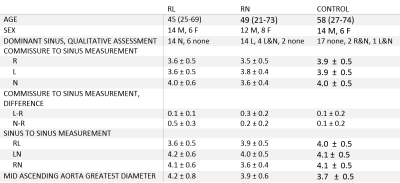
This retrospective IRB approved study queried a database of 735 BAV patients undergoing cardiac MRI and MRA of the thoracic aorta at 1.5T or 3T MRI (Siemens Avanto/Skyra). Aortic valve morphology was classified according to the BAV cusp fusion pattern using ECG gated balanced-steady state free precession (b-SSFP) cines or magnitude phase contrast MR images. Aortic valve stenosis or regurgitation (n=376), partial cusp fusion (n=143), absence of raphe (n=55), or unicuspid valves (n=1) were excluded. For the remaining 160 patients, 20 with right-left coronary cusp fusion BAV [n=135] and 20 with right-non coronary cusp fusion BAV [n=25]) were randomly selected. Additionally, a control group of 20 subjects with tricuspid aortic valves undergoing surveillance for aortic dilation and without significant valvular dysfunction were evaluated. To obtain an orthogonal view of the aortic root, multiplanar reformat of the aortic root was performed on the ECG gated high resolution contrast enhanced MRA (CEMRA) (TE/TR= 1ms/2.7 ms) or from the ECG gated respiratory-navigated 3D inversion recovery SSFP MRA (TE/TR= 1.3 ms/384 ms). The presence of a dominant cusp-sinus was qualitatively noted and quantitatively measured from each sinus to the opposing commissure (Figure 1). To assess sinus dominance in a single subject, the sinus to commissure measurements were subtracted by the value of the right sinus to commissure measurement. This subtraction was done for the left sinus to commissure (left minus right; L-R) and non-coronary sinus to commissure (non minus right; N-R). The diameters of the Sinus of Valsalva (sinus to sinus) and of the mid ascending aorta were also obtained.Results
Table 1 summarizes demographics and aortic measurements. In the BAV patient groups, qualitative assessment found the predominant sinus was located on the opposing side of the conjoined cusp in most subjects (n=14 for right-left fusion; n=14 for right-non fusion group). In the control group, most subjects (n=17) did not show a dominant cusp-sinus. Figure 2 shows boxplots of the commissure to sinus measurement. The L-R and N-R sizes were compared using a Wilcoxon rank-sum test. In the right-left fusion BAV group, the N-R measurements were statistically larger (p<0.001 ), indicating a larger non-coronary cusp in this group. In the right-non fusion BAV group, the L-R measurements were statistically larger (p=0.006), indicating a larger left cusp. In patients with tricuspid aortic valve, the N-R and L-R measurements were not significantly different (p=0.16).Discussion
This study demonstrated an asymmetric shape of the sinus of Valsalva in the majority of the BAV patients. A larger non coronary cusp-sinus was seen in patients with right-left fusion BAV and a larger left cusp-sinus was encountered in patients with right-non fusion BAV, while no cusp predominance was seen in patients with tricuspid aortic valve. The presence of an asymmetric root with eccentric sinus dilation could provide further evidence for the hemodynamic hypothesis, provided it corresponds with the eccentric jets arising from the conjoined cusp region. We postulate that the presence of a predominant sinus on the opposing side of the cusp fusion may be associated with abnormal transvalvular flow.Conclusion
Our study demonstrated the presence of an asymmetric aortic root in patients with right-left and right-non fusion BAV with evidence of a larger sinus size on the opposing side of the conjoined cusp. This finding could inform future studies investigating the role of genetics or hemodynamics in the development of aortopathy.Acknowledgements
No acknowledgement found.References
1. Michelena HI, Della Corte A, Prakash SK, et al. Bicuspid aortic valve aortopathy in adults: Incidence, etiology, and clinical significance. International journal of cardiology 2015;201:400-407
2. Schaefer BM, Lewin MB, Stout KK, et al. The bicuspid aortic valve: an integrated phenotypic classification of leaflet morphology and aortic root shape. Heart 2008;94:1634-1638
3. Verma S, Siu SC Aortic Dilatation in Patients with Bicuspid Aortic Valve. N Engl J Med 2014;370:1920-9. DOI: 10.1056/NEJMra1207059
Figures