3331
Myocardial microvascular dysfunction in patients with end-stage renal disease and the risk factors for the heart damage in hemodialysis1West China Second University Hospital, Chengdu, China, 2West China Hospital, Sichuan University, Chengdu, China
Synopsis
Cardiovascular disease is the major cause of death in patients with chronic kidney disease, this study prospectively enrolled 67 patients with ESRD to quantify evaluate the difference in left ventricular (LV) regional myocardial microvascular function using cardiac magnetic resonance (CMR), and to discuss the factors that may affect myocardial damage in the clinical treatment. The results confirmed that the first-pass perfusion CMR can early defect the myocardial deformation and dysfunction in ESRD patients, and the treatment time may be a risk factor for the cardiovascular disease in the patients with CKD.
Background
Cardiovascular disease is the major cause of death in patients with chronic kidney disease (CKD), the hemodialysis is the major treatment tool for the disease[1-2], and there are multiple factors in the development of cardiovascular disease in patients with ESRD, for example the hypercholesterolemia, hypertension and chronic inflammation, et al. It has been shown the myocardial fibrosis is existed in patients with ESRD undergoing hemodialysis [3].However, the characteristic of myocardial microvascular dysfunction in end-stage renal disease (ESRD) has not been well described and the risk factors were uncertain about the dialysis [4]. In this study we sought to investigate the features of myocardial microvascular dysfunction of patients with ESRD using first-pass perfusion imaging on cardiovascular magnetic resonance (CMR), and further to discuss the factors that may affect myocardial damage in the clinical treatment.Methods
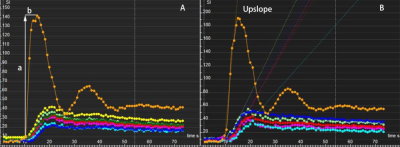
In total, 67 patients with ESRD free of coronary heart disease or diabetes mellitus and 29 healthy subjects were prospectively included and underwent CMR cine and first-pass perfusion examination. The ESRD patients were divided into two groups including 16 patients with systolic dysfunction (EF<50%), and 51 patients with preserved systolic function (EF≥50%). Time for the therapy, clinical symptoms and biochemical variables were detailed recorded. The LV regional myocardial perfusion parameters included upslope, time to maximum signal intensity (TTM) and max signal intensity (MaxSI) were calculated and compared, respectively. The relative risk for heart failure including renal function were recorded and analyzed. Continuous variables were compared using independent Student’s t-test or one-way analysis of variance (ANOVA).Results
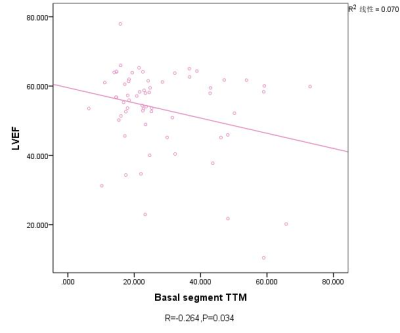
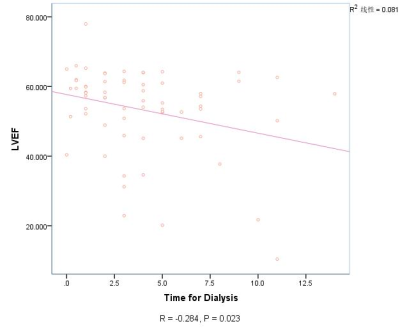
In the ESRD patients with impaired LVEF, we observed significantly higher LVEDV and LVESV than that of the normal controls (p < 0.001). The ESRD patients with impaired LVEF had a significantly lower SV than that of the normal subjects, but the LV mass were markedly increased as compared with the normal controls (all p < 0.001). In the basal, mid- and apical segment, MaxSI reduced significantly in ESRD patients when compared with the normal subjects (all p < 0.001). In contrast to the patients with ESRD and preserved EF, the patients with ESRD and impaired EF had lower upslope in the basal segment (2.53±1.21 vs. 2.04±0.81) and the controls had greater upslope in the mid- segment (3.34 ± 1.29 vs. 2.60 ± 1.07) (all p < 0.05). A significant correlation was observed between first-pass perfusion TTM on basal-segment (r =-0.264, P=0.035), and the SV was correlated with the diagnosis time with the kidney disease (r =-0.273, P=0.029) and the treatment time for the dialysis (r =-0.310, P=0.012).Heart failure occurred in 31 patients (46%) within 1 year, and LV mass and MaxSI were determined as independent risk factor.Conclusion
First-pass perfusion imaging of cardiac magnetic resonance identifies myocardial microvascular dysfunction of patients with ESRD, and high risk of heart failure is evident in these patients.Acknowledgements
This study has received funding by the Program for New Century Excellent Talents in University (No: NCET-13-0386) and Program for Young Scholars and Innovative Research Team in Sichuan Province (2017TD0005) of China.References
[1] Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, McAlister F, Garg A. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17:2034–2047.
[2]Parnham S, Gleadle JM, Bangalore S, et al.Impaired Myocardial Oxygenation Response to Stress in Patients With Chronic Kidney Disease. J Am Heart Assoc. 2015, 4(8):e002249.
[3] Losi MA, Memoli B, Contaldi C, et al.Myocardial fibrosis and diastolic dysfunction in patients on chronic hemodialysis. Myocardial fibrosis and diastolic dysfunction in patients on chronic haemodialysis. Nephrol Dial Transplant. 2010n;25(6):1950-4.
[4] Parnham S, Gleadle J, De Pasquale C, Selvanayagam J. Myocardial ischemia assessment in chronic kidney disease: challenges and pitfalls. Front Cardiovasc Med. 2014;1:1–5.
Figures