3263
Evaluation of tumor shape features for overall survival prognosis in glioblastoma multiforme patients1Department of Biomedical Engineering, National University of Singapore, Singapore, Singapore, 2Department of Neurosurgery, National Neuroscience Institute, Singapore, Singapore
Synopsis
We evaluated 13 shape features of glioblastoma multiforme (GBM) tumor for overall survival (OS) prognosis in 75 patients using univariate and multivariate Cox regression analysis. Age and Karnofsky performance scale were used as covariates for the multivariate analysis. Three shape features were found to be significant for OS prognosis in GBM patients. Kaplan-Merier survival curves were obtained for the significant features to illustrate their effectiveness. In future works, these shape features can be used along with volumetric and texture features derived from the tumor for OS prediction of GBM patients.
Introduction
Age, Karnofsky performance scale (KPS), extent of resection, and the degree of necrosis as well as enhancement of the tumor on pre-operative MR image studies have been found to be prognostic of overall survival (OS) in glioblastoma multiforme (GBM) patients1. In previous studies2, some shape features have also been found to be prognostic of OS in GBM patients. Shape features quantify various aspects of tumor surface irregularities (an irregular tumor surface is associated with poor prognosis). In this work, we study the effectiveness of 13 GBM tumor shape (3D and 2D) features for OS prognosis of GBM patients. 12 out of 13 shape features used in this work have been analyzed for OS prognosis for the first time.Method
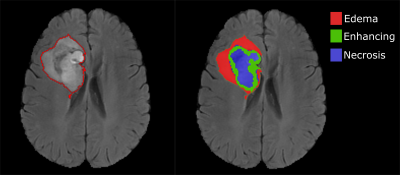
FLAIR MR images of 75 patients obtained from the BraTS 2017 dataset were used in this study3,4. The shape features were extracted from the FLAIR mask (consisting of enhancing tumor, necrosis, and edema regions (refer Figure-1)).
3D tumor shape features
1. Bounding ellipsoid volume ratio (BEVR):
BEVR2 is an indicator of the tumor shape irregularity. It is the ratio of the tumor volume to the volume of the Minimum Volume Bounding Ellipsoid (MVBE) enclosing the tumor5.
2. MVBE orientation:
Angles of rotation of the major, intermediate and minor axes of the MVBE were computed from the rotation matrix of the MVBE of the tumor. The rotation matrix is obtained from the ellipsoid information matrix5.
3. Spherical Disproportion (SD) and Sphericity(SP):
SD and SP are measures of the roundness of the tumor region. 1 <= SP and SD <= 0. For a perfectly spherical object, SP, SD = 1. These features were computed using the Pyradiomics6 package.
2D tumor shape features7
Mean Radial Distance (MRD), Radial Distance Standard Deviation (RDSD), Mass Circularity (MC), Entropy of radial distance (Entropy), Area Ratio (AR), Zero Crossing Count (ZC) and Mass Boundary Roughness (MRB) were extracted from the largest axial slice of the FLAIR mask.
Statistical analysis
Univariate Cox regression analysis was performed for all 2D and 3D shape features individually. The Hazard ratios (HR) and its 95% confidence interval (CI), Wald statistic value (w), and p-value obtained, were used to determine whether a feature is significant for GBM OS prognosis. The shape features found to be significant from the univariate analysis were analyzed using multivariate Cox regression with patient age and KPS as covariates.
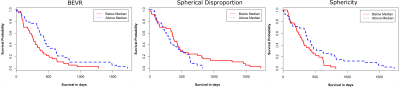
Kaplan-Meier (KM) curves were obtained for the features which were found to be significant from both univariate and multivariate Cox regression analysis, in order to illustrate their effectiveness in OS prognosis of GBM patients. For each shape feature, two patient groups were generated based on the median value of the feature in consideration. Subsequently, each group’s survival curve was observed.
Results and Discussion
The results of the univariate and multivariate Cox regression analysis are shown in Figure-2 and Figure- 3 respectively. None of the 2D shape features evaluated in this study were found to be significant for OS prognosis in GBM patients. Mass circularity, entropy of radial distance, and zero crossing count had p-values <0.05 (Figure-2). However, the 95% CI of their HR included the value 1.0, which indicates that the OS prognosis by the feature is poor. Hence, these features were not considered to be significant. Bounding Ellipsoid Volume Ratio, Spherical Disproportion and Sphericity had p-value < 0.05 and high Wald statistic value from both univariate and multivariate Cox regression analysis (Figure 2 and 3). Figure-4 shows the KM survival curves for the features found to be significant from both univariate and multivariate Cox regression analysis. High BEVR and sphericity values indicate that the tumor has less irregularities. Thus, GBM patients whose tumor masks result in BEVR and sphericity value above the median value for the population are expected to survive longer. In case of spherical disproportion, the inverse should be true, as low spherical disproportion indicates less irregularities. The observations from Figure 4 confirms this hypothesis.Conclusion
This work assessed 2D and 3D shape features derived from the FLAIR abnormality region. BEVR was found to be prognostic of OS in GBM patients, which is consistent with the findings by Czarnek2. Of the 12 shape features being used in this context for the first time, sphericity and spherical disproportion were found to be significant in OS prognosis of GBM patients. In future works, we aim to integrate these shape features with other features (such as texture, clinical, volumetric etc.) to predict the OS of GBM patients.Acknowledgements
This work is supported by the Singapore Academic Research Fund under Grant R-397-000-227-112, NUSRI China Jiangsu Provincial Grant BK20150386 BE2016077 and NMRC Bedside Bench under grant R-397-000-245-511 awarded to Dr. Hongliang Ren. This research is also supported by the Singapore Ministry of Health’s National Medical Research Council under its Translational and Clinical Research Flagship Program- Tier 1 (Project No: NMRC/TCR/016-NNI/2016).References
- Lacroix, Michel, et al. "A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival." Journal of neurosurgery 95.2 (2001): 190-198.
- Czarnek, Nicholas, et al. "Algorithmic three-dimensional analysis of tumor shape in MRI improves prognosis of survival in glioblastoma: a multi-institutional study." Journal of neuro-oncology 132.1 (2017): 55-62.
- Bakas, Spyridon, et al. "Advancing The Cancer Genome Atlas glioma MRI collections with expert segmentation labels and radiomic features." Scientific data 4 (2017): 170117.
- Menze, Bjoern H., et al. "The multimodal brain tumor image segmentation benchmark (BRATS)." IEEE transactions on medical imaging 34.10 (2015): 1993-2024.
- Moshtagh, Nima. "Minimum volume enclosing ellipsoid." Convex Optimization 111 (2005): 112.
- Griethuysen Joost, et al. “Computational Radiomics System to Decode the Radiographic Phenotype”. Accepted Cancer Research 2017.
- Georgiou, Harris, et al. "Multi-scaled morphological features for the characterization of mammographic masses using statistical classification schemes." Artificial Intelligence in Medicine 41.1 (2007): 39-55
Figures