3214
Is ADC Affected by Distortion of EP-DWI for Distinguishing Parotid Gland Tumor- To Compare ADC of Parotid Gland in Echo-Planar DWI and PROPELLER DWI1Master 's Program of Biomedical Informatics and Biomedical Engineering, Feng Chia University, Taichung City 407, Taiwan, 2Department of Automatic Control Engineering, Feng Chia University, Taichung City 407, Taiwan, 3Ph. D. Program of Electrical and Communications Engineering, Feng Chia University, Taichung City 407, Taiwan, 4Department of Radiology, Tri-Service General Hospital, Taipei, Taiwan, 5Department of Diagnostic Radiology, The University of Hong Kong, Hong Kong, Hong Kong, 6Ph.D. program of Technology Management, Chung Hua University, Hsinchu, Taiwan, 7Department of Medicine, Taipei Medical University, Taipei, Taiwan, 8Department of Dentistry, National Defense Medical Center, Taipei, Taiwan, 9Department of Radiology, National Defense Medical Center, Taipei, Taiwan, 10Master 's Program of Biomedical Informatics and Biomedical Engineering, Feng Chia University, TAICHUNG, Taiwan, 11Institute of Automatic Control Engineering, Feng Chia University, TAICHUNG, Taiwan
Synopsis
The study is to investigate if the perceptible geometric distortions could bias for parotid pleomorphic adenomas (PMA) by ADC measurements by comparing PROPELLER-DWI with EP-DWI. This retrospective study enrolled 14 PMAs. All participants underwent 1.5-T fat-saturated diffusion-weighted imaging with PROPELLER-DWI and EP-DWI. ADCs were measured on normal parotid gland and PMA for PROPELLER-DWI and EP-DWI. Our results showed that PMAs had significantly higher ADC than normal parotid glands no matter on PROPELLER-DWI or EP-DWI. The ADC measured by PROPELLER-DWI was significantly higher than by EP-DWI, but they were proportional to each other. EP-DWI allows distinguishing PMAs even under image distortion.
Introduction
Diffusion-weighted magnetic resonance (MR) imaging has widely been applied to explore the water diffusion of the parotid glands using apparent diffusion coefficient (ADC) calculations in humans since 2001.1-3 The wide variation in ADC measurements, even in healthy volunteers : 0.28 × 10ˉ³ mm2/s to 2.46 × 10ˉ³ mm2/s,4,5 consequently makes the interexperimental comparisons of parotid ADCs difficult. Such discrepancy has been partly attributed to the different strengths (b values)6, nonaccelerated and accelerated echo-planar diffusion-weighted sequences, fat-saturated and nonfat-saturated, and PROPELLER diffusion-weighted imaging sequences7. Compared to single shot EP-DWI, PROPELLER-DWI is less distortion and has also been applied to healthy parotid glands to reduce geographic distortion and chemical shift artifacts in 20097. However, if the perceptible geometric distortions could bias for distinguishing parotid tumor by ADC measurements, it has never been investigated before. In this study, we explored this problem by ADC measurements in single shot EP-DWI and PROPELLER DWI.Materials and Methods
MR scan: A total of 14 patients who had the pleomorphic adenomas (PMA) and received both PROPELLER-DWI and EP-DWI were enrolled. All MR scans were performed at a 1.5 T whole-body scanner (GE Healthcare, Signa HDx, US) using an 8NV head and neck array coil. DWI images were obtained with motion-probing diffusion gradients (b factors, 0 and 1000 sec/mm2) applied in each of three orthogonal directions. For PROPELLER-DWI, fast spin-echo sequences (TR/TE/NEX=7000/76/1.8) were performed with fat saturation by using an echo train length of 24, as described by Pipe et al7. For same scan time with PROPELLER-DWI, EP-DWI acquisitions (TR/TE/NEX=7000/73.3/4) were performed without acceleration. Data analysis: All MR data were digitally transferred from the MR unit console to a personal computer and processed with software developed in house by using Matlab (MathWorks, Natick, MA). Imaging quality, including imaging distortion, signal-to-noise ratio (SNR), and contrast-to-noise ratio (CNR), of PROPELLER-DWI and EP-DWI were evaluated quantitatively. On PROPELLER-DWI and EP-DWI, one slice containing the largest area of the parotid tumor and another slice containing the largest area of contralateral parotid gland were used for quantitative data analysis in each tumor, respectively. ADC maps were generated by using a pixel-by-pixel computation according to the following logarithmic equation: ADC = ln(SI0/SI1000)/(b1000 - b0), where SI0 and SI1000 were signal intensities of the DWI obtained with b values of 0 sec/mm2 (b0) and 1000 sec/mm2 (b1000), respectively. Mean ADCs of all pixels within ROI were used for comparison between PROPELLER-DWI and EP-DWI. Statistical analysis: Statistical analysis was performed by using SPSS 12.0 (SPSS, Chicago, III) software. Wilcoxon signed-rank test and Mann-Whitney U test were used for comparison. A P value less than 0.05 was considered as statistically significant.Result
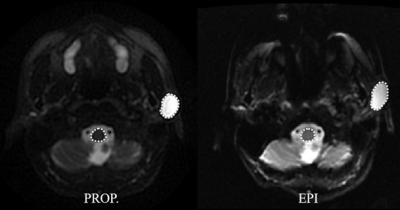
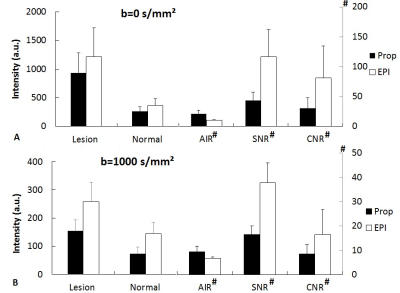
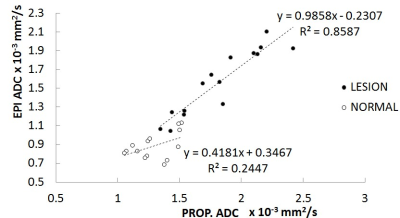
A case demonstration of imaging distortion on PROPLLER-DWI and EP-DWI and ROIs was shown on Fig. 1. Fig. 2 illustrated the signal intensity of parotid tumor (Tumor), normal parotid gland (Normal), air background (Air), SNR, and CNR between PROPELLE-DWI and EP-DWI. ADC of tumor and normal parotid glands measured by PROPELLER-DWI and EP-DWI was illustrated on Fig. 3. The ADCs of pleomorphic adenomas were 1.82 ± 0.34 (×10ˉ³ mm2/s) and 1.57 ± 0.24 (×10ˉ³ mm2/s) for PROPELLER-DWI and EP-DWI, respectively. The ADCs of normal parotid gland were 1.30 ± 0.17 (×10ˉ³ mm2/s) and 0.89 ± 0.14 (×10ˉ³ mm2/s) for PROPELLER-DWI and EP-DWI, respectively. The ADC measured by PROPELLER-DWI was significantly higher than that measured by EP-DWI. PMAs had significantly higher ADC than normal parotid glands no matter on PROPELLER-DWI or EP-DWI (P<0.01). Fig. 4 plotted the scatter diagram in a ROI of ADCs on normal and tumor region between PROPELLE-DWI and EP-DWI, and the correlation coefficients were r=0.93 and 0.49, respectively.Discussion
Our results showed that PROPELLER-DWI had significantly lower SNR and CNR than EP-DWI within same scan time. The reason is partly attributed to the lower NEX in PROPELLER-DWI (NEX=1.8) than EP-DWI (NEX=4). Our results are consistent with a prior study7, showing significantly higher ADC of normal parotid glands in PROPELLER-DWI than in EP-DWI. Although the distinct ADC between PROPELLER-DWI and EP-DWI, they are proportional to each other at both of normal and tumor region. Moreover, both of them can differentiate the PMA from normal parotid gland.Conclusion
Even though ADC might be affected by distortion in EP-DWI measurement, it does not obstruct the performance of differential diagnosis in parotid tumor.Acknowledgements
The study was supported partly from the Ministry of Science and Technology, R. O. C. under the Grant No. MOST 105-2221-E-035 -049 -MY2 and 105-2314-B-016 -024 -MY2.References
1. Wang J, Takashima S, Takayama F, et al. Head and neck lesions: characterization with diffusion-weighted echo-planar MR imaging. Radiology. 2001;220(3):621-30.
2. Eida S, Sumi M, Sakihama N, Takahashi H, Nakamura T. Apparent diffusion coefficient mapping of salivary gland tumors: prediction of the benignancy and malignancy. AJNR Am J Neuroradiol. 2007;28(1):116-21.
3. Habermann CR, Arndt C, Graessner J, et al. Diffusion-weighted echo-planar MR imaging of primary parotid gland tumors: is a prediction of different histologic subtypes possible? AJNR Am J Neuroradiol. 2009;30(3):591-6.
4. Sumi M , Takagi Y , Uetani M, et al.. Diffusion-weighted echoplanar MR imaging of the salivary glands. AJR Am J Roentgenol 2002;178:959–965
5. Zhang L , Murata Y , Ishida R , Ohashi I , Yoshimura R , Shibuya H. Functional evaluation with intravoxel incoherent motion echo-planar MRI in irradiated salivary glands: a correlative study with salivary gland scintigraphy. J Magn Reson Imaging 2001;14:223–229.
6. Thoeny HC , De Keyzer F , Boesch C , Hermans R. Diffusion-weighted imaging of the parotid gland: influence of the choice of b-values on the apparent diffusion coefficient value. J Magn Reson Imaging 2004;20:786–790.
7. Juan CJ, Chang HC, Hsueh CJ, et al. Salivary glands: echo-planar versus PROPELLER Diffusion-weighted MR imaging for assessment of ADCs. Radiology. 2009;253(1):144-52.
Figures