3212
Development of Diffusion Tensor Imaging to Assess Traumatic Peripheral Nerve Injury and RecoveryMichael Pridmore1, Wesley P. Thayer2, Mark Does3, and Richard Dortch4
1Institute of Imaging Science, Vanderbilt University, Nashville, TN, United States, 2Plastic Surgery, Vanderbilt University Medical Center, Nashville, TN, United States, 3Biomedical Engineering, Vanderbilt University, Nashville, TN, United States, 4Radiology and Radiological Sciences, Vanderbilt University Medical Center, Nashville, TN, United States
Synopsis
Current clinical management following traumatic peripheral nerve injuries (TPNI) and repair require physicians to rely on qualitative measures from patient history/physical exam that can cause delay in patient care. Such delays can a negative impact on outcomes because the healing of nerves must occur in a timely fashion to avoid permanent loss of sensory and/or motor function. The current study aims to test the feasibility of performing DTI measurements in TPNI patients to better improve clinical outcomes.
Purpose
Presently, clinical management following traumatic peripheral nerve injuries (TPNI) and repair requires physicians to “wait and watch” for months to years and rely on qualitative measures from patient history/physical exam. These delays have a negative impact on outcomes because re-innervation must occur in a timely fashion to prevent permanent loss of sensorimotor function. Previous work has shown that DTI of the distal nerves of the wrist is feasible and reports on myelin and axon pathologies [1-4]. The long-term aim of this project is to employ DTI in the median and/or ulnar nerves of patients following TPNIs as a quantitative, early measure of nerve regeneration. The current study aims to i) test the sensitivity of performing DTI in a cross-section of TPNI patients and ii) acquire preliminary longitudinal data to determine the ability of DTI to monitor recovery.Methods
Subjects: Three TPNI patients with various injuries had their injured arm scanned approximately three months after surgical repair (see Table 1). Each subject’s uninjured arm was scanned during the same session and served as an internal control. One subject (Patient 3) returned for a follow-up scan 3 months after the surgery. Data acquisition: Subjects were imaged with a 3.0-T Philips Achieva MR scanner. An 8-channel wrist coil was used for RF reception in all subjects expect one, where a larger 16-channel knee coil was used due to a cast covering the arm. High-resolution, single-shot DTI scan was performed at a slice thicknesses of 4-mm with 10 slices in each subject. Additional parameters included: resolution = 0.75x0.75x4 mm3 (wrist coil acquisitions) or 1.25x1.25x8 mm3 (knee coil acquisitions), TR/TE = 3000/53 ms, averages = 12, 16 diffusion directions, max b-factor of 800 s/mm2, and scan time ≈ 11 minutes. Data analysis: Image registration/tensor estimation was performed using FSL/CAMINO [5]. Regions of interest (ROIs) were manually selected on all slices for the median and ulnar nerves, and mean slice-wise fractional anisotropy (FA) values were estimated. In addition, the ∆FA between the injured and uninjured nerve was estimated in proximal and distal to the injury site (Table 2). Finally, fibertracking results were accomplished via CAMINO using seed-points in the most proximal/medial/distal slice, way-points halfway between each seed-point, and a curve/FA threshold of 20˚/0.2. Given the small sample size and heterogeneity of injury types, we treat each patient as an individual case study in the following analysis.Results
In patient 1, reductions in FA (mean±SD) were found in the injured left-arm median nerve (0.33±0.18) when compared to the median (0.61±0.10) nerve in the right uninjured arm. In patient 2, similar reductions in FA were found in the injured left-arm ulnar nerve (0.30±0.08), while the ulnar nerve in the right uninjured arm was higher (0.42±0.11). In patient 3, reductions in FA were found in both median (0.30±0.05) and ulnar (0.32±0.08) nerves in the injured right arm when compared to the uninjured nerves (median/ulnar:0.54±0.10/0.49±0.12). Patient 3 returned 3-months later for a follow-up scan with similar results for the right injured median (0.33±0.06) and ulnar nerves (0.30±0.09) and the uninjured nerves (median/ulnar:0.64±0.11/.52±0.13). Across all our patients, we found reduced FAs in the injured nerve compared to other nerve in the same injured arm, as well from the uninjured nerves in the other arm. Figure 1 illustrates the FA values we obtained in a representative sample, with injured and noninjured arms compared in proximal and distal slices of the wrist. It should be noted, however, that edema from injury can reduce FA at the injury site. Additional existing challenges in this protocol were i) choosing a suitable coil that minimized discomfort and fit around large casts and ii) positioning of our participants during scanning (currently prone with arm above head), which had an impact on scan time. Preliminary fibertracking results comparing an injured median nerve to the uninjured median nerve in the same patient can be shown on Figure 2. Note the continuous fiber tracts in the uninjured median nerve, and the termination of the fiber tracts in the injured median nerve at the site of injury.Discussion and Conclusions
DTI in the distal nerves of the wrist is feasible and sensitive to TPNI. Further work will focus on i) obtaining data in a larger cohort of patients and matched controls; ii) refining the scan protocol, specifically with coil selection and subject position on the table; and iii) tracking patients over the period of one year to determine the ability of DTI to track change over time. Methods that model edema will also be investigated along with fiber tracking methods to visualize nerve regeneration over time.Acknowledgements
R01 NS097821, MR 150075, W81-XWH-15-JPC-8/CDRMP-NMSIRA, and T32 EB014841-05 for fundingReferences
[1] Guggenberger, et al. Radiol 265:194-203 (2012). [2] Heckel, et al. PLoS ONE 10(6):e0130833 (2015). [3] Stein, et al. J Magn Reson Imag 29:657-662 (2009). [4] Zhou, et al. J Magn Reson Imag 36(4):920– 927 (2012). [5] Soares, et al. Front Neurosci. 7:31(2013).Figures
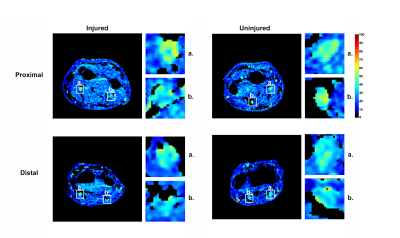
Figure 1: FA maps proximal (top) and distal (bottom) to the wrist shown for the injured
and noninjured nerve data (left) for a representative sample (Patient 2) with a
left arm ulnar nerve injury. Median (a.) and ulnar nerve (b.) squared and
zoomed in for detail. 2 of 10 slices shown.
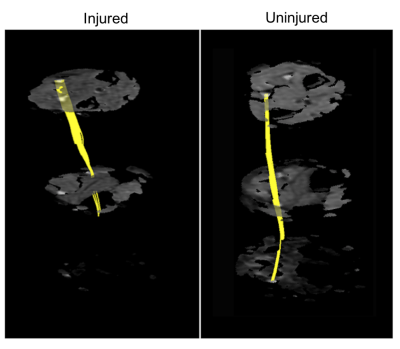
Figure 2:
Fibertracking results of representative sample (Patient 3, timepoint 1) for the
injured median nerve (left-side), compared to the same patient’s uninjured
median nerve in the other arm (right-side). Slices are ordered from proximal
(top) to distal (bottom).
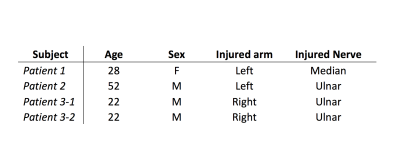
Table 1: Descriptive statistics for each patient, including age, sex,
and type of injury.
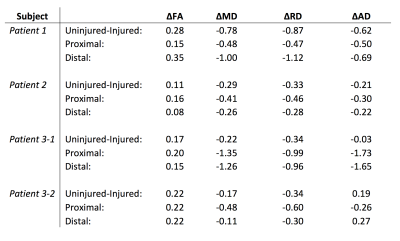
Table 2: Difference (Δ) of uninjured and injured
nerve diffusion values: Fractional Anisotropy (FA), Mean Diffusivity (MD: μm2/ms),
Radial Diffusivity (RD: μm2/ms), and Axial Diffusivity (AD: μm2/ms). Diffusivity values
proximal and distal to each patient’s respective injury site are also reported.