3202
Diffusional kurtosis imaging of parotid glands in Sjögren's syndrome: Initial findings1Department of Radiology, Drum Tower Hospital, School of Medicine, Nanjing University, Nanjing, China, 2Philips Healthcare, Shanghai, Shanghai, China
Synopsis
A total of 40 patients with SS and 40 healthy volunteers underwent DKI-MR imaging, which generated ADC, D, and K values. The MR nodular grade was determined on the basis of MR morphological findings. The parotid ADC, D, and K values in patients with SS were significantly higher than those of healthy volunteers. The K values correlated positively with the MR nodular grade significantly in patients with SS.All parotid DKI parameters differed significantly among patients with SS at different MR nodular grades. Parotid DKI parameters hold great potential in diagnosing SS, especially in early-stage SS without MR morphological changes.
INTRODUCTION
Primary Sjögren’s syndrome (pSS) is a chronic autoimmune disease with a direct injury to exocrine glands . The objective diagnostic evidence of pSS includes serological, ocular, salivary, and labial gland histopathological tests. The salivary tests include salivary flow measurement, x-ray sialography, and technetium-99m pertechnetate scintigraphy. X-ray sialography is a classical examination, yet with invasiveness and radiation exposure. Currently, magnetic resonance imaging (MRI) have been proved to be superior to x-ray sialography in evaluating parotid parenchymal noninvasively. Although DWI is now widely used in multiple areas, it generates apparent diffusion coefficient (ADC) values by using a monoexponential model, which assumes the Gaussian behavior of water molecule diffusion. In this study, we explored the application of diffusion kurtosis imaging (DKI) MR imaging that quantifies the non-Gaussian behavior of water molecule diffusion in characterize the features of parotid glands in patients with Sjögren's syndrome (SS).METHODS
A total of 40 patients with SS and 40 healthy volunteers underwent 3.0T magnetic resonance imaging (MRI) including DKI, which generated the apparent diffusion coefficient (ADC), corrected diffusion (D), and diffusional kurtosis (K) values. The MR nodular grade was determined on the basis of MR morphological findings. usion kurtosis imaging (DKI) MR imaging that quantifies the non-Gaussian behavior of water molecule diffusion in characterize the features of parotid glands in patients with Sjögren's syndrome (SS).RESULTS
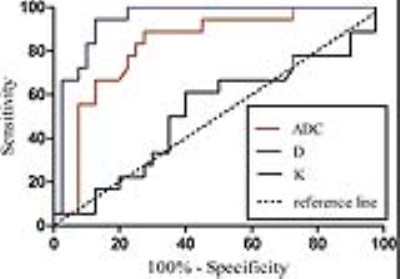
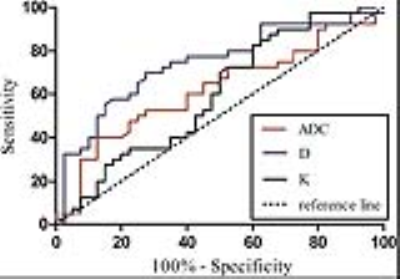
The parotid ADC, D, and K values in patients with SS were significantly higher than those of healthy volunteers (P = 0.011, < 0.001, 0.022, respectively). The parotid ADC and D values in patients with SS of MR nodular grade 0 were significantly higher than those of healthy volunteers (all P < 0.001). The parotid D value showed an accuracy of 75.0% and 87.9% in diagnosing patients with SS and MR nodular grade 0, respectively. The parotid ADC and D values correlated negatively, while the K values correlated positively with the MR nodular grade significantly in patients with SS (r = -0.741, -0.605, 0.424, all P < 0.001). All parotid DKI parameters differed significantly among patients with SS at different MR nodular grades (all P < 0.001).DISCUSSION
In this study, the D values were significantly higher than the ADC values in both healthy volunteers and patients with SS. The increased parotid D and ADC values might be involved with lymphocyte infiltration, gland edema, and increased vascular permeability, causing enlarged extracellular space and increased water molecular diffusion, especially in the early-stage SS.1, 2 Meanwhile, the D and ADC values of parotid glands with MR nodular grade 0 were significantly higher than those with grades 1, 2, and 3. The parotid D and ADC values in patients with SS conversely correlated with the MR nodular grade (from grade 0 to 3) significantly. We speculated that as the disease progressed, the glandular parenchyma was destroyed and underwent atrophy and fibrosis, leading to a restricted water molecule diffusion and decreased D and ADC values.
The K value is a unitless parameter representing a measure of the extent to which tissue diffusion deviates from a Gaussian pattern and could reflect the heterogeneity of the microenvironment in the gland.3,4 The parotid K values in patients with SS were significantly higher than those in healthy volunteers (a difference rate of 5.9%). Even in patients with SS, the K values of the parotid gland with MR nodular grade 2 were significantly higher than those with grade 0, and the parotid K values of grade 3 were significantly higher than those with both grades 0 and 1. Moreover, the parotid K value correlated positively with the MR nodular grade (from grade 0 to 3) significantly in patients with SS. It might be speculatedthat as the parotid injury aggravated accompanied with increased fat deposition, inflammation components, and fibrotic tissues, the microenvironmental complexity increased, leading to an increased kurtosis deviating fromthe Gaussian distribution of extracellular water molecule diffusion.
Among multiple DKI parameters, the parotid D value showed the highest accuracy of 75.0% in diagnosing SS, which was higher than those of the parotid ADC and K values. Since a close monitoring and targeted diagnostic approach are needed by patients with SS for a long time, the parotid DKI parameters could serve as quantitative and specific indexes in the long-term follow-up for patients with SS.
CONCLUSION
Parotid DKI parameters hold great potential in diagnosing SS, especially in early-stage SS without MR morphological changes.Acknowledgements
No acknowledgement found.References
1. Xuan J, Shen L, Malyavantham K, et al. Temporal histological changes in lacrimal and major salivary glands in mouse models of Sjogren’s syndrome. BMC Oral Health 2013;13:51.
2. Mavragani CP, Moutsopoulos HM. The geoepidemiology of Sjogren’s syndrome. Autoimmun Rev 2010;9:A305–A310.
3. Rosenkrantz AB, Sigmund EE, Johnson G, et al. Prostate cancer: feasibility and preliminary experience of a diffusional kurtosis model for detection and assessment of aggressiveness of peripheral zone cancer. Radiology 2012;264:126–135.
4.Rosenkrantz AB, Sigmund EE, Winnick A, et al. Assessment of hepatocellular carcinoma using apparent diffusion coefficient and diffusion kurtosis indices: preliminary experience in fresh liver explants. Magn Reson Imaging 2012;30:1534–1540.
Figures