3185
MR Myelo-Neurography: Improved Visualization of MR Neurography in the Brachial Plexus using a Combination of SHINKEI and Phase-Cycling balanced SSFP1Department of Radiological services, Tokyo Women’s Medical University Hospital, Tokyo, Japan, 2Department of Diagnostic Imaging & Nuclear Medicine, Tokyo Women’s Medical University Hospital, Tokyo, Japan, 3Philips Electronics Japan, Tokyo, Japan
Synopsis
The brachial plexus could be involved in various kinds of diseases, which may lead to serious functional disorders. MR neurography is a useful technique for evaluating the abnormal state of the peripheral nerves, however, it is still difficult to visualize the entire brachial plexus, including nerve roots, using conventional MR neurography due to its complicated anatomical structure. In this study, we evaluated a new MR neurography using a combination of SHINKEI and Phase-Cycling balanced SSFP sequence to visualize the entire brachial plexus.
INTRODUCTION
There are various techniques for MR neurography,1-3 which is a useful method for visualization of the brachial plexus. Imaging interpretation of nerve roots is also important when deciding surgical procedures in some cases, such as traumatic brachial plexus injuries and neonatal brachial plexus palsy (NBPP). However, it is still difficult to visualize both the brachial plexus and nerve roots using conventional MR neurography.4,5 On the other hand, evaluation of cervical nerve roots using constructive interference in the steady state (CISS) has been reported,6 however, it is difficult to visualize the brachial plexus on CISS. Phase-Cycling balanced SSFP (c-SSFP) is a technique to reduce band artifacts using phase cycling as well as CISS; two consecutive runs of 3D balanced steady-state free precession with different phase angles are performed internally and subsequently combined.7 Therefore, a combination of MR neurography and c-SSFP would be promising for improving the depiction of the nerves entire the brachial plexus, but it can be required long scan time and does not fit a routine time slot. Recently, Compressed-SENSE (CSENSE), which is a combination of compressed sensing and SENSE, has been developed as a new method to shorten acquisition time with minimum image quality deterioration. Thus, we proposed a new technique, MR Myelo-Neurography (MRMN), which combined SHINKEI MR neurography3 with c-SSFP using CSENSE, to visualize both the brachial plexus and nerve roots within a feasible scan time.Methods
Visualization of the brachial plexus and nerve roots was evaluated in six healthy volunteers (6 males aged 29-43 years.) using 3T MR unit. (Ingenia 3T, Philips Healthcare R5.1.7)
Theory:
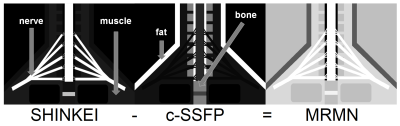
MRMN is a subtraction technique, and obtains two images: SHINKEI and c-SSFP. (Figure 1) The brachial plexus shows high signal intensity on SHINKEI; however, it is still not enough to demonstrate nerve roots because the signal intensity of nerve roots is similar to the signal intensity of cerebral-spinal fluid and an acquisition time must be extended to provide sufficient image quality. Conversely, c-SSFP excellently demonstrates nerve roots though it is difficult to visualize the brachial plexus because the brachial plexus and surrounding muscles show similar signal intensities. Therefore, on MRMN, we suggested that images on SHINKEI and c-SSFP were subtracted to emphasize signal intensity of both the brachial plexus and nerve roots.
imaging parameters:
c-SSFP can be combined with CSENSE to shorten acquisition time. Imaging parameters of SHINKEI and c-SSFP were as follows: slice orientation = coronal, SHINKEI: TR/TE = 2400 / 61ms, FOV = 220(FH)*220(RL)*70(AP) mm, Voxel size = 1.0*1.0*1.0mm, SENSE factor = 2.0, Total acquisition time = 3:40. c-SSFP: TR/TE = 6.0 / 2.5ms, FOV = 220(FH)*134(RL)*70(AP) mm, Voxel size = 0.48*0.48*0.48mm, CSENSE factor = 1.5, Total acquisition time = 4:55.
Results
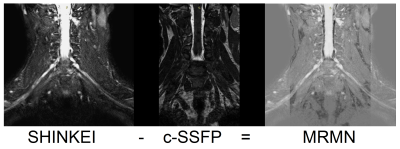
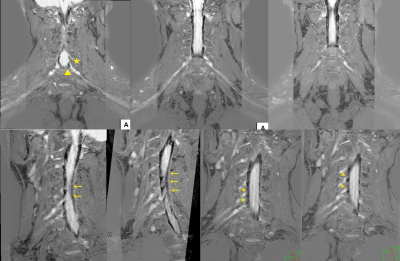
On MRMN, signal intensity of both the brachial plexus and nerve roots were emphasized more strongly than background signals, such as muscles, and both the brachial plexus and nerve roots were clearly visualized in all subjects. (Figure 2) Dosal and ventral roots were clearly distinguished from each origin. (Figure 3, 4)Discussion
We have reported a modified technique, HIRE-SHINKEI to visualize the peripheral nerves in the pelvis.8 It was based on a subtraction technique, which subtracts two images with SHINKEI and 3D-heavily-T2W to suppress signal intensity of the long-T2 areas in the background. As a result, signals of the nerves are emphasized on HIRE-SHINKEI. 3D-heavily-T2W can also depict nerve roots, however, it requires significantly extended acquisition time to demonstrate nerve roots with sufficient image quality. c-SSFP can also visualize nerve roots without extension of acquisition time unlike 3D-heavily-T2W. CSENSE is also useful in shortening acquisition time without image quality deterioration. Therefore, a combination of SINEKI and c-SSFP with CSENSE clearly showed both the brachial plexus and nerve roots within feasible acquisition time.Conclusion
MRMN clearly demonstrates the whole brachial plexus, and could be a helpful method to contribute to the diagnosis of nerve root and peripheral nerve disorders.Acknowledgements
No acknowledgement found.References
1: Filler AG, et al. Application of magnetic resonance neurography in the evaluation of patients with peripheral nerve pathology. J Neurosurg. 1996 Aug;85(2):299-309.
2: Du R, et al. Magnetic resonance neurography for the evaluation of peripheral nerve, brachial plexus, and nerve root disorders. J Neurosurg. 2010 Feb;112(2):362-71.
3:Yoneyama M, et al. Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci. 2013;12:111-9.
4: Somashekar D, et al. High-resolution MRI evaluation of neonatal brachial plexus palsy: A promising alternative to traditional CT myelography. AJNR Am J Neuroradiol. 2014 Jun;35(6):1209-13.
5: Yoshikawa T, et al. Brachial plexus injury: clinical manifestations,conventional imaging findings, and the latest imaging techniques. Radiographics. 2006 Oct;26 Suppl 1:S133-43. 5
6: Vargas MI, et al. New approaches in imaging of the brachial plexus. Eur J Radiol. 2010 May;74(2):403-10.
7:Deimling M, et al. Book of Abstracts, chapter Constructive interference in steady state (CISS) for motion sensitivity reduction, page842. Society of Magnetic Resonance in Medicine, 1989. 43-3.
8: Tadenuma H, et al. : Proceedings of the 25th Annual Meeting of ISMRM (2017).
Figures