3006
The Characteristics of Chronic Internal Carotid Artery Occlusion for Successful Endovascular Intervention by 3D MR Vessel Wall Imaging1Radiology, Renji hospital, Shanghai Jiaotong University, Shanghai, China, 2Neurosutgery, Renji hospital, Shanghai Jiaotong University, Shanghai, China, 3Philips Healthcare, Shanghai, China, 4Biomedical Engineering & Center for Biomedical Imaging Research, Tsinghua University, Beijing, China, 5Radiology, University of Washington, Seattle, WA, United States
Synopsis
Visualization of the extent and components of internal carotid artery chronic total occlusion (CTO) may play an important role in deciding whether patients can undergo the endovascular intervention successfully or not. This study sought to investigate the characteristics of internal carotid artery CTO for successful endovascular intervention by 3D MR Vessel Wall Imaging. We found that patients with lower extent of occlusion and IPH at the proximal occlusion site had a higher success rate of recanalization. The results suggest 3D MR vessel wall imaging might be useful of patient selection for more possibly successful endovascular intervention.
Introduction
Endovascular recanalization in patients with carotid chronic total occlusion (CTO) has been reported to be technically challenging[1]. The patient selection criteria for the treatment of CTO are currently decided by conventional intra-arterial digital subtraction angiography (DSA). 3D MR vessel wall imaging techniques have been developed to accurately visualize and quantify both the lumen and the vessel wall components of large arteries[2]. In this study, we retrospectively analyzed the pre-procedural 3D MR vessel wall imaging in patients with internal carotid artery CTOs and its relationship to technical success rates.Methods
Study Sample: Patients who were diagnosed and confirmed with internal carotid artery CTOs by ultrasound or conventional CT angiography were included in the study.MR imaging: 3D vessel wall images were acquired using a whole body clinical scanner (Philips Achieva TX, the Netherlands) and a dedicated 8-channel phased-array carotid coil. 3D vessel wall sequences were acquired with the following parameters: (1)3D MERGE: the improved motion-sensitized driven-equilibrium (iMSDE) prepared rapid gradient echo sequence[3], TR/ TE 9.3/4.4 ms, flip angle 6°, FOV 250[FH] ×160[RL]×64[AP] mm3, acquisition matrix 312×200×80, acquired resolution 0.8×0.8×0.8mm3, Rec resolution 0.4×0.4×0.4mm3, acquisition time 2 minutes 42 seconds; (2) 3D SNAP[4]: phase sensitive Inversion recovery enabled 3D inversion recovery turbo field echo, TR/TE 10/4.8 ms, flip angle 11°, field of view 160×32×160mm3, spatial resolution 0.8×0.8×0.8mm3, and scan time 2min 17sec.Endovascular recanalization: The patients subsequently underwent endovascular recanalization within 1 week of the 3D MR vessel wall imaging. Patients were divided into two groups according to technical success or not of the endovascular recanalization. Data analysis: An experienced radiologist reviewed the carotid vessel wall images. The morphologic characteristics regarding left side lesion, the stump conditions, occlusion site over C2 segment, intraplaque hemorrhage (IPH) at the proximal occlusion site and residual true lumen visibility in C1 segment were recorded.Results
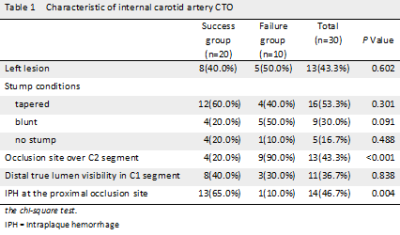
A total of 30 patients (25 men; age: 60.8 years old; range: 42 to 72 years) were included in the final statistical analysis. 20 patients underwent successful recanalization. Table 1 summarized the characteristics of internal carotid artery CTOs on 3D MR vessel wall images. There was no difference of lesion side between success group and failure group (40% vs 50%; P=0.602). The stump conditions and distal true lumen visibility in C1 segment appeared no significant different between the two groups(all P>0.05). However, Identified by MR vessel wall images, the success group exhibit less prevalence of occlusion site over C2 segment as well as higher prevalence of IPH at the proximal occlusion site compared with the failure group(20.0% vs 90%,P<0.001; 65.0% vs. 10.0%,P=0.004).Discussion and conclusions
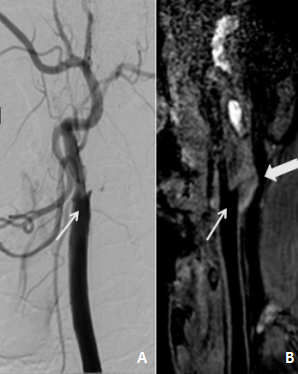
Our study investigated the characteristics of internal carotid artery CTO on 3D MR vessel wall images between successful and failure recanalization. Our results showed that the patients with occlusion site limited to C2 or below and IPH over start part of occlusion had a higher success rate of recanalization. Visualization of the extent of internal carotid artery CTO by 3D MR vessel wall imaging not only provides clear reference for wiring procedure, but also implies lumen patency in distal segment. When the distal internal carotid artery is reconstituted at levels distal to C2 segment, the difficulty of guide wire manipulation may increase. Meanwhile, 3D MR vessel wall imaging has the advantage for determine the compositions of the proximal cap. Interestingly, the success rate in occlusions with IPH in our analysis was in fact higher. The potential reason is that IPH may actually provide a roadmap, and thus facilitate wiring procedures. Our study had several limitations including its small sample size, and other factors (such as the length of time the vessel was occluded or the hemodynamic status) were not evaluated. In conclusion, our findings indicate that 3D MR vessel wall imaging may play a role in patient selection of endovascular recanalization in patients with carotid CTO, and this potential benefit should be proven to outweigh the risk of procedural complication in further investigations.Acknowledgements
None.References
[1]. Kwak, J.H., et al., The Outcome and Efficacy of Recanalization in Patients with Acute Internal Carotid Artery Occlusion. American Journal of Neuroradiology, 2012.35(4): p. 747-753.
[2]. Ying Cai., et al., Atherosclerotic plaque features and distribution in bilateral carotid arteries of asymptomatic elderly population: A 3D multicontrast MR vessel wall imaging study. European Journal of Radiology 96 (2017) 6–11
[3]. Wang J, Börnert P, Zhao H et al (2013) Simultaneous non-contrast angiography and intraplaque hemorrhage (SNAP) imaging for carotid atherosclerotic disease evaluation. Magn Reson Med 69:337–345
[4]. Obara M, Van Cauteren M, Honda M, Imai Y, Kuroda K. Assessment of improved motion-sensitized driven equilibrium (iMSDE) for multi-contrast vessel wall screening. Magn Reson Med Sci. 2014;13:139–144.
[5]. Chen, Y., et al., Predictors for Successful Endovascular Intervention in Chronic Carotid Artery Total Occlusion. JACC: Cardiovascular Intervention, 2016.9(17): p. 1825-1832.
[6]. Lee, C., et, al., Predicting procedure successful rate and 1-year patency after endovascular recanalization for chronic carotid artery occlusion by CT angiography. Vol.221.2016.772-776.
[7]. Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. J Am Coll Cardiol Intv 2011;4: 213–21.
Figures