3004
High prevalence of intraplaque hemorrhage in peripheral artery disease is indicated by large coverage femoral vessel wall MRI1Radiology, University of Washington, Seattle, WA, United States, 2Vascular Surgery, University of Washington, Seattle, WA, United States, 3Cardiology, University of Washington, Seattle, WA, United States
Synopsis
Intraplaque hemorrhage (IPH) is known to be a high-risk atherosclerotic plaque feature based on carotid imaging but its prevalence is unknown in peripheral artery disease (PAD). Since PAD is a diffuse disease that can occur along a long stretch of the femoral artery, large coverage 3D vessel wall MRI is required to identify IPH prevalence in PAD. This study reports the high prevalence of IPH in patients with an abnormal ankle-brachial index (ABI) using IPH specific large coverage 3D vessel wall MRI.
Introduction
Peripheral artery disease (PAD) caused by reduced blood supply to lower limb muscles secondary to femoral atherosclerosis is a functionally debilitating disease and leads to secondary cardiovascular events. Early detection of high-risk PAD atherosclerosis may allow better management strategies. Studies using vessel wall MRI in other arteries have shown that presence of T1 hyperintensity, indicative of intraplaque hemorrhage (IPH), denotes a high-risk plaque phenotype with rapid progression and early-onset clinical complications [1,2]. However, previous studies using limited coverage 2D vessel wall MRI have found minimal to no IPH in PAD [3,4]. Since PAD is a diffuse disease, the limited arterial coverage in previous studies may not represent the true prevalence of IPH.Aim
To estimate the prevalence of intraplaque hemorrhage in PAD using large-coverage 3D vessel wall MRI.Methods
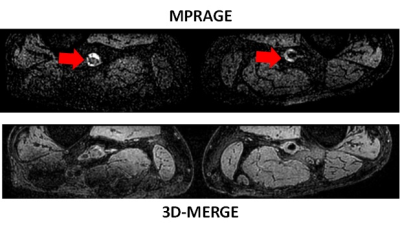
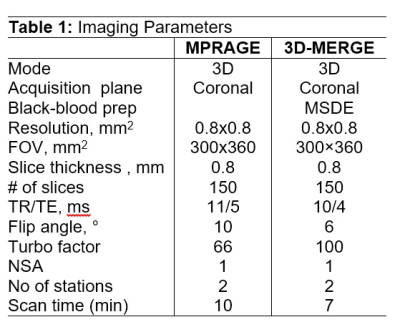
MR Imaging: Twelve patients (68.4±7.7 years, 75% male) were scanned on a Philips Achieva 3T scanner with torso phased array coil under local IRB guidelines and informed consent. All subjects recruited had ABI<0.9 in at least one leg (mean ABI 0.77). After a three-plane survey and time-of-flight angiogram to locate the femoral arteries, 3D MPRAGE sequence to provide information about IPH or thrombosis was acquired in the coronal orientation. The scan was performed in two stations with overlap between stations to cover the entire femoral artery from the common femoral bifurcation to below the popliteal junction. Then a 3D black-blood sequence (3D-MERGE [5]) with the same isotropic resolution and scan geometry as MPRAGE was performed. After gadolinium contrast (Prohance or Gadovist, 0.1mmol/kg dose at 1cc/sec), 3D-MERGE was repeated 5 minutes post-injection. Imaging parameters are provided in Table 1. Image Analysis: Multi-station 3D images scanned in coronal orientation were fused into a large field-of-view coronal 3D volume. MPRAGE, pre and post contrast 3D-MERGE were reviewed together using multi-planar reformatting to axial views. Intraplaque hemorrhage/thrombus (IPH/T) was detected by referring hyperintensity to adjacent muscles consistent with previous studies in carotid and coronary arteries. Corresponding reformats on pre-contrast and post-contrast 3D-MERGE were reviewed to classify the IPH/T as IPH (located within vessel wall) or Thrombus (located within lumen). Location (proximal thigh, mid-thigh, popliteal), laterality (unilateral or bilateral) and number of lesions per artery were also assessed. A representative case of IPH with corresponding axial reformats is shown in Figure 1.Results
Coverage of the femoral artery from the common femoral artery bifurcation to the popliteal artery was obtained with good image quality. IPH/T was present in 8 out of 12 (66%) subjects. Among subjects with IPH/T, 4 had bilateral IPH/T (50%), all but one subject had IPH/T at multiple locations (88%). An example of bilateral IPH is shown in Figure 2. All patients with IPH/T had a mid-thigh lesion in the adductor canal region except one subject who had proximal thigh involvement without a mid-thigh lesion. Two subjects had diffuse IPH/T extending the length of the adductor canal to the popliteal region and these were counted as one lesion each in the mid-thigh and popliteal segments. Discrete multiple IPH lesions were observable in other subjects and were counted individually. Based on this, the IPH/T distribution of 24 IPH/T lesions was proximal thigh 29%, mid-thigh 58% and popliteal 13%. The mean longitudinal extent of an IPH/T lesion was 7.1mm (range 1.5mm – 30mm). Based on co-registered black-blood images, all lesions except a single thrombus in the proximal thigh of one patient, were classified as IPH.Discussion
This is the first vessel wall MRI study to focus on IPH in PAD. Prior studies covering a short segment of the femoral bifurcation indicated a low prevalence of IPH [3,4]. Using large coverage MRI, a high prevalence of IPH was observed in this study, with multiple lesions per subject with the majority occurring in the mid-thigh adductor canal region. Co-registration with black-blood sequences suggests that the T1 hyperintense signal corresponds to IPH rather than thrombus. The adductor canal is known to be subject to frequent mechanical stress [6] and the high prevalence of IPH in the adductor canal may be a consequence of this repeated trauma. Whether IPH may also play a significant role in more rapid PAD progression and ischemic complications, as documented in carotid atherosclerosis, requires further evaluation in prospective longitudinal studies using large coverage MRI.Conclusions
Utilizing large coverage 3D MRI, we found a high prevalence (66%) of femoral IPH/thrombus in PAD in patients with an ABI<0.9. Co-registered black-blood MRI suggests that the T1 hyperintense signals are intramural corresponding to IPH. IPH in PAD most commonly occurs in the mid-thigh region in the adductor canal.Acknowledgements
No acknowledgement found.References
[1] Saam T, Hetterich H, Hoffmann V, et al. Meta-analysis and systematic review of the predictive value of carotid plaque hemorrhage on cerebrovascular events by magnetic resonance imaging. J Am Coll Cardiol 2013; 62:1081-1091.
[2] Noguchi T, Kawasaki T, Tanaka A, et al. High-Intensity Signals in Coronary Plaques on Noncontrast T1-Weighted Magnetic Resonance Imaging as a Novel Determinant of Coronary Events. J Am Coll Cardiol 2014; 63:989-999.
[3] Polonsky TS, Liu K, Tian L, Carr J, Carroll TJ, Berry J, Criqui MH, Ferrucci L, Guralnik JM, Kibbe MR, Kramer CM, Li F, Xu D, Zhao X, Yuan C, McDermott MM. High-risk plaque in the superficial femoral artery of people with peripheral artery disease: prevalence and associated clinical characteristics. Atherosclerosis. 2014 Nov;237(1):169-76.
[4] Li F, McDermott MM, Li D, Carroll TJ, Hippe DS, Kramer CM, Fan Z, Zhao X, Hatsukami TS, Chu B, Wang J, Yuan C., The association of lesion eccentricity with plaque morphology and components in the superficial femoral artery: a high-spatial-resolution, multi-contrast weighted CMR study. J Cardiovasc Magn Reson. 2010 Jul 1;12:37.
[5] Balu N, Yarnykh VL, Chu B, Wang J, Hatsukami T, Yuan C., Carotid plaque assessment using fast 3D isotropic resolution black-blood MRI. Magn Reson Med. 2011 Mar;65(3):627-37.
[6] Brown R, Nguyen TD, Spincemaille P, Prince MR, Wang Y, In vivo quantification of femoral-popliteal compression during isometric thigh contraction: Assessment using MR angiography. J Magn Reson Imaging. 2009 May;29(5):1116-24.
Figures