2985
Central thoracic vein imaging without Gadolinium: diagnostic confidence of DANTE-based 3D subtractive NCE-MRA and comparison with 2D bSSFP1Radiology, Addenbrooke's Hospital and University of Cambridge, Cambridge, United Kingdom
Synopsis
Imaging of the central thoracic veins is often challenging due to renal failure and/or difficult venous access, which render contrast agent administration problematic. This work assesses a non-contrast-enhanced free-breathing 3D subtractive MR angiography method for thoracic central vein imaging in a group of 18 patients. Evaluation by experienced radiologists demonstrated that angiograms obtained with this new method give high diagnostic confidence, which is significantly better than our standard 2D breath-hold approach in the absence of contrast medium. There is also better agreement between readers for the new sequence.
Introduction
Imaging of the central thoracic veins can be valuable in patients with suspected central venous stenosis, occlusion or thrombus, allowing diagnosis of pathology or identification of safe and reliable routes for deep venous access. MR is especially important for assessing the superior vena cava (SVC) and innominate veins which cannot reliably be imaged with ultrasound. Administration of Gadolinium-containing contrast agents is often difficult or inappropriate: this patient group often has poor venous access, and up to half of patients referred at our institution have substantial renal impairment. Our clinical practice in these cases has been to acquire breath-hold 2D bSSFP images but these scans are often non-diagnostic or have poor diagnostic confidence. This study aims to assess whether the diagnostic confidence of non-contrast-enhanced (NCE) central vein imaging can be improved by using a free-breathing 3D subtractive MR angiography method, and whether it affects the radiologist’s diagnosis.Methods
Following ethical approval and informed consent, 18 patients were recruited following clinical referral for thoracic venography. They were imaged on a 1.5 T Discovery MR450 system (GE Healthcare, Waukesha, WI) using a 16-channel anterior cardiac array and the in-built posterior spine array. Our standard clinical 2D breath-hold bSSFP series (2D-BH) were first acquired (TE/TR=1.9/4.4 ms, acquisition matrix 256 x 256, FoV 40 cm, slice thickness 4mm) in oblique coronal orientation.
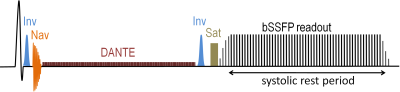
Vascular MR images were acquired in coronal orientation using a 3D free-breathing navigator-gated subtractive NCE angiography pulse sequence (3D-NavNCE)1 shown schematically in Figure 1. Bright- and dark-blood images were acquired sequentially, with blood signal suppressed using DANTE2 (TR 1 ms, flip angle 10°, gradient 20 mT/m, ETL 110–150 pulses). The image readout was a segmented balanced SSFP with acquisition matrix 256×256, flip angle 65°, TE/TR=1.1/2.8 ms, FoV 40 cm, 20–32 slices of 4 mm, ASSET factor 3, shot TR 2 heartbeats. Each k-space plane was acquired over 2 shots, and each shot began with 10 sinusoidally increasing dummy acquisitions. The image readout (duration 120ms) was placed during the end-systolic cardiac rest period to avoid cardiac motion. Fat signal was suppressed dual inversion-recovery1 and out-of-slab signal was suppressed using spatial pre-saturation. A cylindrical respiratory navigator (acceptance window 3–4 mm) was used to reduce respiratory motion artifacts.
The 2D-BH and 3D-NavNCE datasets were were anonymised separately and reviewed separately by two experienced vascular radiologists, in random order and blinded to all other patient information. Seven venous segments were assessed: superior vena cava (SVC), and left and right innominate (LI, RI), subclavian (LS, RS) and internal jugular (LJ, RJ) veins. Each vessel was assessed for the presence of stenosis/occlusion (scale 0–5: 0=no stenosis, 5=complete occlusion) and for the diagnostic confidence (scale 0–4: 0=non-diagnostic, 4=excellent) in this assessment.
Confidence scores were compared using the paired sample Wilcoxon signed rank test, with a significance level of p<0.05. Data for each reviewer was treated separately. Pathology scores were compared for diagnosis of significant stenosis (>50%, scores 3–5). Agreement between the two methods and between the two reviewers was assessed as percentage of agreeing segments and as a Cohen’s Kappa.
Results
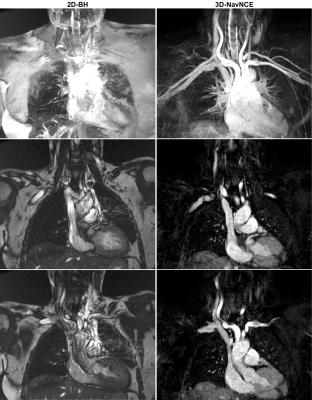
Figure 2 shows 3D-NavNCE and 2D-BH images for an example patient.
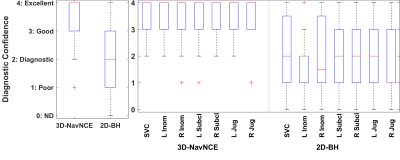
Figure 3 shows boxplots of the diagnostic confidence scores for each method, both separated by vessel type and with all vessels grouped together. For every vessel and reviewer, the diagnostic confidence was significantly greater for the 3D-NavNCE sequence.
Method agreement: the pathology diagnoses for the two methods (from reviewer 1 / reviewer 2) were in agreement for 78%/75% of vessel segments, with Cohen’s Kappa values of 53%/52% indicating only moderate agreement between of the two methods for diagnosis of significant stenosis.
Reviewer agreement: the two reviewers were in agreement over the diagnosis of significant stenosis for 87% of vessel segments for 3D-NavNCE but only 73% of segments for 2D-BH. The corresponding Cohen Kappa values were 73% (good agreement) for 3D-NavNCE and 49% (moderate agreement) for 2D-BH.
Discussion and Conclusion
The 3D-NavNCE sequence gives primarily excellent (score 4) or good (score 3) images of the thoracic vasculature, which our radiologists feel confident to report from and strongly prefer to the 2D-BH method which was previously our only sequence for evaluation of patients unsuitable for contrast-agent administration. In addition to its value for highlighting stenosis, this method is also expected to be better at distinguishing thrombus from flowing blood.
Only ten patients in this cohort were able to receive contrast-enhanced MRA; therefore we have not yet evaluated the diagnostic accuracy of this method. If successfully validated against contrast-enhanced MRA, the new method would be valuable for the majority of patients referred at our centre, who have either renal failure or difficult vascular access.
Acknowledgements
We thank the NIHR Cambridge Biomedical Research Centre and Addenbrooke’s Charitable Trust for funding this work.References
1. Comparison of DANTE- and iMSDE-based methods for subtractive NCE-MRA of the central thoracic veins, AN Priest, KH Mortensen, DJ Lomas, Proc Intl Soc Mag Reson Med. 2015;23:2662.
2. Li L, Miller KL, Jezzard P. DANTE-prepared pulse trains: a novel approach to motion-sensitized and motion-suppressed quantitative magnetic resonance imaging. Magn Reson Med. 2012 Nov;68(5):1423–38.
Figures