2968
Left Atrial Surface Strain from Cine MRI Data in Patients with Mitral Regurgitation1Auburn University MRI Research Center, Auburn University, Auburn, AL, United States, 2Department of Electrical and Computer Engineering, Auburn University, Auburn, AL, United States, 3Division of Cardiovascular Disease, University of Alabama at Birmingham, Birmingham, AL, United States
Synopsis
Mitral regurgitation (MR) is a common form of valvular disease where degeneration of the mitral valve causes blood from the left ventricle to be regurgitated into the left atrium (LA). For some MR patients, surgery to repair or replace the mitral valve is an option, but it can be difficult to determine when to do the surgery. Volumetric remodeling in the left atrium in MR patients has been
Purpose
Mitral regurgitation (MR) is a common form of valvular disease where degeneration of the mitral valve causes blood from the left ventricle to be regurgitated into the left atrium (LA). For some MR patients, surgery to repair or replace the mitral valve is an option, but it can be difficult to determine when to do the surgery. Volumetric remodeling in the left atrium in MR patients has been reported, and could precede remodeling of the left ventricle (LV) and damage to the LV wall. Here, we investigate changes in endocardial surface strain in the LA in patients with MR compared to normal volunteers.Methods
Population/Imaging protocol: MRI was acquired from 8 normal subjects (age 19-24) and 10 patients (age 48-82) with isolated MR. Both groups were imaged with standard cardiac cine slices with a 2-chamber and a 4-chamber view, and a stack of short-axis (SA) views covering both atria. Parameters were set as follows: FOV: 360-400mm, 8mm slice thickness, no gap, 256*256 matrix. Contouring and Surface Fitting: Endocardial contours were manually drawn at ventricular end diastole (ED) and end systole (ES) continuously in each slice containing the atrium. Intersections of the mitral annulus (MA) with the LV wall were manually placed in 2 and 4-chamber views at end diastole (ED) and end systole (ES). All intersections and endocardial contours were propagated to the remaining time frames using automated algorithm1. Circles were fit to the mitral annuli based on the MA/2-chamber, 4-chamber intersections and used to determine which contour points were part of the LA. Closed triangular surfaces were fit to LA contours by constructing a subject-specific template, then propagated it to the remaining timeframes a previously reported algorithm2. Deformation Analysis: The triangulated surface has an approximate vertex-to-vertex correspondence over time, and 3D displacement field was derived from the surface by measuring the displacement of each vertex. LV endocardial surface strain at the centroid of each triangle was computed from the displacements of the corresponding triangle vertices using the atrial maximum volume point as reference. A validation of this technique is presented in a separate abstract. A segmental model for the LA was constructed, where the LA was divided into three levels: proximal, medial, and distal to the MA. In each level, the model was further segmented into anterior, posterior, septal and lateral segments. For each segment, the median strain was recorded. Strains in the MR and normal groups were comparted using a student’s t-test.Results
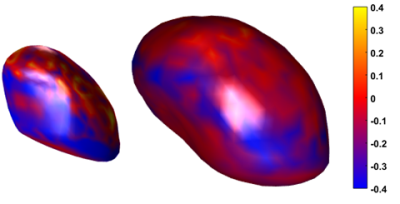
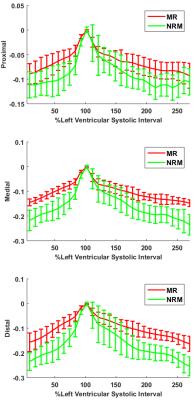
Figure 1 shows LA endocardial surfaces of a representative MR patient and normal volunteer colored with minimum principal surface strain at ventricular ED. Figure 2 shows averaged LA minimum principal surface strain for MR patients and normal subjects across a cardiac cycle. As Figure 2 shows, MR has higher strains in all three levels, which demonstrates reduced LA myocardium contraction in MR patients. A comparison of the minimum principal surface strains at the LA maximum volume phase is displayed in Figure 3. Significant differences were found in the medial and distal layers for LA between the normal subjects and MR patients.Discussion
Changes in LA volume and function may be useful in determining the severity and chronicity of valvular regurgitation, and may help inform treatment decisions such as timing of valve surgery. The endocardial LA surface strain versus time in Figure 2 shows that LA contracts less in MR, which is consistent with previous results from LA volumetric and surface curvature analysis2.Conclusion
Atrial deformation can be derived from cine MRI data. In MR patients, in addition to LA enlargement3, there are changes in LA deformation. This finding has clinical potential in optimizing surgery timing and patient management.Acknowledgements
No acknowledgement found.References
1. Feng W, Nagaraj H, Gupta H, et al. A dual propagation contours technique for semi-automated assessment of systolic and diastolic cardiac function by CMR. J Cardiovasc Magn Reson. 2009 Aug 13;11:30.
2. Zhang X, S. Lloyd, et al. Four Chamber Endocardial Surface Reconstruction from Cardiac MRI Data, ISMRM, 2017, 3156
3. Zhang X, S, Lloyd, et al. Left Atrial Enlargement and Systolic Failure Measured By Cardiac MRI In Severe Isolated Mitral Regurgitation With Preserved Left Ventricular Ejection Fraction, ISMRM, 2017, 2868
Figures