2926
The impact of left ventricular ejection fraction on cardiovascular blood flow1Linköping University, Linköping, Sweden
Synopsis
The impact of left ventricular (LV) ejection fraction (LVEF) on cardiovascular blood flow is not completely understood. We used a method, called “Atlas heart generation”, to investigate cardiovascular flow of patients with ischemic heart disease (n=62). The patients underwent 4D-Flow MRI and were stratified according to LVEF. We found that the lower LVEF group had lower velocities throughout the aorta, in a portion of LV and left atrium, at peak-systole. At early-diastole, differences were observed in the aortic arch, and in the apical-septal segments of LV. The suggested method can detect changes in cardiovascular flow and add to pathophysiological understanding.
Introduction
Left ventricular systolic function is commonly evaluated by left ventricular ejection fraction (LVEF). Although a reduced LVEF is accompanied with altered cardiovascular blood flow [1], a low LVEF cannot in itself characterize the ensuing changes in the local blood flow characteristics. A comprehensive assessment of cardiovascular blood flow and its relation to LVEF might provide further insight into pathophysiological mechanisms and have additional diagnostic and prognostic values. 4D Flow MRI enables non-invasive measurement of three-dimensional, time-resolved blood flow and has been used to assess healthy and diseased hearts in earlier studies. We recently developed a method called “atlas heart generation”, which enables analysis of 4D Flow MRI data of a group of patients together [2]. The purpose of this study is to utilize this approach to investigate the effect of left ventricular systolic function on aortic and intra-cardiac blood flow in male patients with suspected or diagnosed ischemic heart disease (IHD).Methods
62 male patients with suspected or diagnosed IHD underwent MRI at 3T. The protocols included 4D Flow and morphological imaging. The morphological images were acquired with retrospective cardiac gating (spatial resolution:1.0x1.0x8.0mm3, temporal resolution:30ms, flip angle:45°, TR:2.8ms, TE:1.4ms). The 4D Flow data were acquired during free breathing with respiratory gating (VENC:120cm/sec, flip angle:10°, TR:4.4ms, TE:2.6ms, spatial resolution:2.7x2.7x2.8mm3, SENSE:3). LVEF was calculated using morphological images and the patients were stratified into two groups according to their LVEF; lower LVEF group (LVEF:43±10) and higher LVEF group (LVEF:69±4), respectively. 4D velocity magnitude atlases and standard deviation maps of the stratified groups were derived using the atlas heart generation method [2]. Briefly, an average heart was created using the images of patients treated with a non-rigid registration method. The individual patients were then non-rigidly registered to the average heart which reduces the anatomical differences between patients while retaining the blood flow patterns. The 4D velocity maps of stratified groups were compared by p-value maps which are 4D statistical maps comparing groups at each voxel and at each time frame by student t-test.Results
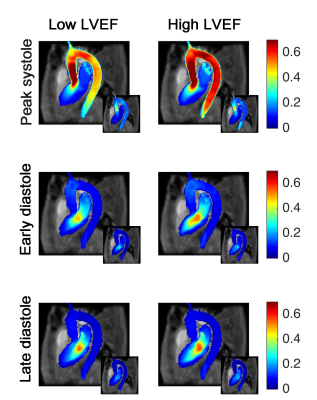
No differences were observed in age (66±6 vs. 67±7, p=0.96), BMI (29±5 vs. 27±4, p=0.37) and heart rate (72±12 vs. 72±14, p=0.99) between the lower and higher LVEF groups. Figure-1 displays the maximum intensity projection of velocity atlas and the standard deviation map for the low and high LVEF groups at peak-systole, early-diastole and late-diastole. The mean velocity was lower for the low LVEF group in thoracic aorta (0.41±0.10 vs. 0.51±0.08m/s, p<0.001), in the LV (0.16±0.02 vs. 0.19±0.03m/s, p<0.001), and in the LA (0.12±0.02 vs. 0.14±0.01m/s, p<0.001) at peak-systole, but only in the LV (0.16±0.05 vs. 0.19±0.05m/s, p=0.04) at early diastole.
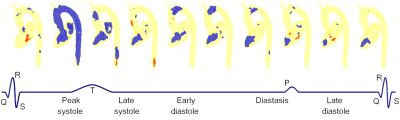
Figure-2 shows the p-value maps comparing low and high LVEF groups. At peak-systole, the low LVEF group had lower velocity in 90% of the thoracic aorta, 46% of the LV and 44% of the LA. At late-systole, the low LVEF group had lower velocities in the LV (44%) and the LA (31%). At early-diastole, the low LVEF group retained lower velocities only in a portion of the aortic arch (12%), and the LV (33%). The lower velocity volume in the LV was located mostly near the intraventricular septum, slowly diminishing through diastasis towards the apical area.
Discussion
The atlas heart generation method enabled comparison of cardiovascular blood flow between different patients locally. In contrast to analysis methods used in previous studies, in which cardiovascular blood flow analysis was performed by oversimplifying 4D Flow data to a single or a few parameters per chamber, this approach represents full four-dimensional flow dynamics. The atlases and standard deviation maps provided information about the expected flow patterns, range of values and the variability within the patients with/without reduced LVEF. We found that in the low LVEF group, the flow towards aorta as well as the flow throughout the mid and apical segments of LV were significantly reduced. The abnormally low mid and apical blood flow distribution was retained in the LV until diastasis in the low LVEF patient group.Conclusion
In this study, we utilize the atlas heart generation method to compare local blood flow characteristics between groups with different LV systolic function. We found significant differences in the whole thoracic aorta, in the vicinity of the aortic valve and a portion of the LA at systole, as well as in the LV throughout the entire cardiac cycle. The hemodynamic atlases and p-value maps facilitated the detection of local blood flow and have the potential to add to pathophysiological understanding and diagnosis in the future.Acknowledgements
No acknowledgement found.References
1.Agati L, Cimino S, Tonti G et al. Quantitative analysis of intraventricular blood flow dynamics by echocardiographic particle image velocimetry in patients with acute myocardial infarction at different stages of left ventricular dysfunction. Eur Heart J Cardiovasc Imaging 2014;15(11):1203-1212.
2.Cibis M, Bustamante M, Eriksson J, Carlhall CJ, Ebbers T. Creating hemodynamic atlases of cardiac 4D flow MRI. J Magn Reson Imaging 2017.
Figures