2905
Cardiac MR multi-modal imaging: role in diagnosis and differential diagnosis of fulminant myocarditis in children1Shandong Medical Imaging Research institute, Jinan, China, 2Shandong Provincial Hospital, Jinan, China
Synopsis
Clinical characteristics, cardiac morphology, function parameters and myocardial tissue characterization on MRI of three groups (FM, AM and CM) were retrospectively compared to find that higher myocardial thickness and T2 ratio were seen in FM than in AM and CM with statistical significance; the LVEF and incidence of LGE in FM were higher than that in CM with statistical significance. So that CMR has values in the diagnosis and differential diagnosis of FM.
Objectives: To analyze clinical characteristics, cardiac magnetic resonance (CMR) findings of acute myocarditis (AM), chronic myocarditis (CM) and fulminant myocarditis (FM) in children and to find out the values of CMR in diagnosis and differential diagnosis of FM.
Methods: 44 children with myocarditis were involved in the study and were divided into three groups (AM, n=20; CM, n=11; FM, n=13) according attacking time. Clinical characteristics (including gender, age, heart rate, myocardial enzyme, and clinical symptoms), cardiac morphology (including thickness of inter-ventricular septum and left ventricular end-diastolic dimension (LVEDD)), function parameters (including left ventricular end-diastolic volume (EDV), end-systolic volume (ESV), left ventricular myocardial mass (LV mass), stroke volume (SV), and ejection fraction (LVEF)) and myocardial tissue characterization (including T2 ratio, early gadolinium enhancement (EGE) ratio and late gadolinium enhancement (LGE)) of three groups were compared.
CMR examinations were performed with 3.0‑T systems. The CMR imaging protocols included: 1) cine imaging with balanced steady state free precession (b-SSFP) sequences in three long axis and sequential short axis (SA) from ventricular base to apex; 2) T2-weighted imaging with a triple inversion recovery spin-echo sequence in 4-chamber and SA; 3) early gadolinium enhancement (EGE) with T1-weighted spin-echo sequence in 4-chamber before and after (within 3minutes) an intravenous bolus of 0.1 mmol/kg Gd-DTPA; 4) late gadolinium enhancement (LGE) with 3D phase-sensitive inversion recovery (3D-PSIR) sequence in 4-chamber and sequential SA 7-10 minutes after another injection of 0.1 mmol/kg Gd-DTPA. Inversion time of 3D-PSIR sequence was adjusted to null normal myocardium.
Chi-square test for contingency tables was obtained to detect associations between clinical characteristics of AM, CM and FM. One way analysis of variance (ANOVA) and Kruskal-Wallis test were used to compare the levels of cTnT and BNP, cardiac morphology and function parameters and myocardial tissue characterization (T2 ratio, EGE ratio and LGE) of AM, CM and FM.
Results: The LVEF of FM children at the onset by echocardiography was 38.5±8.7%, which was much lower than that in AM (60.7±7.8%, P<0.001) and CM children (63.3±2.9%, P<0.001). Clinical manifestations in FM group were various. Compared with AM and CM, higher myocardial thickness of FM (median, 9.3mm VS 7.1mm, P=0.017; 9.3mm VS 7.1mm, P=0.009, respectively) and T2 ratio (1.99±0.14 VS 1.77±0.23, P=0.027; 1.99±0.14 VS 1.66±0.26, P=0.002, respectively) were found in FM children. The LVEF (66.9±7.4% VS 56.7±8.4%, P=0.018) and incidence of LGE (11.8% VS 2.7%, P=0.001) in FM children were higher than that in CM children with statistical significance. There were no statistically significant differences between EDV, ESV, SV and LV mass in AM, CM and FM group.
Conclusion: Compared with AM and CM, FM was characterized by various and severe clinical manifestations, higher levels of myocardial enzymes and severer myocardial inflammatory response. CMR has values in the diagnosis and differential diagnosis of FM and is a useful tool to monitor potential myocarditis-related injuries over the course of myocarditis.
Key words: fulminant myocarditis; cardiac magnetic resonance; tissue characterization; differential diagnosis; children
Acknowledgements
Many thanks to the technicians and nurses in our department and the engineers in Simens company. Thank my family for there love and support.References
1. Ginsberg F, Parrillo JE: Fulminant myocarditis. Crit Care Clin 2013 Jul;29:465-483.
2. Caforio AL, Pankuweit S, Arbustini E, Basso C, Gimeno-Blanes J, Felix SB, Fu M, Heliö T, Heymans S, Jahns R, Klingel K, Linhart A, Maisch B, McKenna W, Mogensen J, Pinto YM, Ristic A, Schultheiss HP, Seggewiss H, Tavazzi L, Thiene G, Yilmaz A, Charron P, Elliott PM, European Society of Cardiology Working Group on Myocardial and Pericardial Diseases: Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013;34:2636-2648.
3. Stensaeth KH, Hoffmann P, Fossum E, Mangschau A, Sandvik L, Klow NE: Cardiac magnetic resonance visualizes acute and chronic myocardial injuries in myocarditis. Int J Cardiovasc Imaging 2012;28:327-335.
4. Felker GM, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Baughman KL, Hare JM: Echocardiographic Findings in Fulminant and Acute Myocarditis. J Am Coll Cardiol 2000;36:227-232.
5. McCarthy RE 3rd, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Hare JM, Baughman KL: Long-term outcome of fulminant myocarditis as compared with acute (nonfulminant) myocarditis. N Engl J Med 2000;342:690-695.
6. Amabile N,Fraisse A,Bouvenot J,Chetaille P,Ovaert C: Outcome of acute fulminant myocarditis in children. Heart 2006;92:1269-1273.
7. Cooper LT, Baughman KL, Feldman AM, Frustaci A, Jessup M, Kuhl U, Levine GN, Narula J, Starling RC, Towbin J, Virmani R, American Heart Association, American College of Cardiology, European Society of Cardiology, Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology: The role of endomyocardial biopsy in the management of cardiovascular disease: a scientific statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology. Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. J Am Coll Cardiol 2007;50:1914-1931.
8. Chow LH, Radio SJ, Sears TD, McManus BM: Insensitivity of right ventricular endomyocardial biopsy in the diagnosis of myocarditis. J Am Coll Cardiol 1989;14:915-920.
9. Hauck AJ, Kearney DL, Edwards WD: Evaluation of postmortem endomyocardial biopsy specimens from 38 patients with lymphocytic myocarditis: implications for role of sampling error. Mayo Clin Proc 1989;64:1235-1245.
10. Shirani J, Freant LJ, Roberts WC: Gross and semiquantitative histologic findings in mononuclear cell myocarditis causing sudden death, and implications for endomyocardial biopsy. Am J Cardiol 1993;72:952-957.
11. Bruder O, Schneider S, Nothnagel D, Dill T, Hombach V, Schulz-Menger J, Nagel E, Lombardi M, van Rossum AC, Wagner A, Schwitter J, Senges J, Sabin GV, Sechtem U, Mahrholdt H: EuroCMR (European Cardiovascular Magnetic Resonance) registry: results of the German pilot phase. J Am Coll Cardiol 2009;54:1457-1466.
12. Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT, White JA, Abdel-Aty H, Gutberlet M, Prasad S, Aletras A, Laissy JP, Paterson I, Filipchuk NG, Kumar A, Pauschinger M, Liu P, International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis: Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol 2009;53:1475-1487.
13. Lieberman EB, Hutchins GM, Herskowitz A, Rose NR, Baughman KL: Clinicopathologic description of myocarditis. J Am Coll Cardiol 1991;18:1617-1626.
14. Ramachandra G, Shields L, Brown K, Ramnarayan P: The challenges of prompt identification and resuscitation in children with acute fulminant myocarditis: case series and review of the literature. J Paediatr Child Health 2010;46:579-582.
15. Mahrholdt H, Goedecke C, Wagner A, Meinhardt G, Athanasiadis A, Vogelsberg H, Fritz P, Klingel K, Kandolf R, Sechtem U: Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation 2004;109:1250-1258.
16. Mavrogeni S, Bratis K, Georgakopoulos D, Karanasios E, Kolovou G, Pavlides G, Papadopoulos G: Evaluation of myocarditis in a pediatric population using cardiovascular magnetic resonance and endomyocardial biopsy. Int J Cardiol 2012;160:192-195.
17. Buechel EV, Kaiser T, Jackson C, Schmitz A, Kellenberger CJ: Normal right- and left ventricular volumes and myocardial mass in children measured by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2009; 11:19.
18. Kawel-Boehm N, Maceira A, Valsangiacomo-Buechel ER, Vogel-Claussen J, Turkbey EB, Williams R, Plein S, Tee M, Eng J, Bluemke DA. Normal values for cardiovascular magnetic resonance in adults and children. J Cardiovasc Magn Reson 2015;17:29.
19. Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS, American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging: Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539-542.
20. Lee EY, Lee HL, Kim HT, Lee HD, Park JA: Clinical features and short-term outcomes of pediatric acute fulminant myocarditis in a single center. Korean J Pediatr 2014;57:489-495.
21. Hsiao HJ, Hsia SH, Wu CT, Lin JJ, Chung HT, Hwang MS, Su WJ, Chang YS: Clinical Presentation of Pediatric Myocarditis in Taiwan. Pediatr Neonatol 2011;52:135-139.
22. Freedman SB, Haladyn JK, Floh A, Kirsh JA, Taylor G, Thull-Freedman J: Pediatric myocarditis: emergency department clinical findings and diagnostic evaluation. Pediatrics 2007;120:1278-1285.
23. Robbers-Visser D, Boersma E, Helbing WA: Normal biventricular function, volumes, and mass in children aged 8 to 17 years. J Magn Reson Imaging 2009;29:552-559.
24. Shillcutt SK, Thomas WR, Sullivan JN, Duhachek-Stapelman A: Fulminant myocarditis: the role of perioperative echocardiography. Anesth Analg 2015;120:296-299.
25. Hauser AM, Gordon S, Cieszkowski J, Timmis GC: Severe transient left ventricular "hypertrophy" occurring during acute myocarditis. Chest 1983;83:275-277.
26. Pinamonti B, Alberti E, Cigalotto A, Dreas L, Salvi A, Silvestri F, Camerini F: Echocardiographic findings in myocarditis. Am J Cardiol 1988;62:285-291.
27. Banka P, Robinson JD, Uppu SC, Harris MA, Hasbani K, Lai WW, Richmond ME, Fratz S, Jain S, Johnson TR, Maskatia SA, Lu JC, Samyn MM, Patton D, Powell AJ: Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. J Cardiovasc Magn Reson 2015;17:96.
28. Olimulder MA, van Es J, Galjee MA: The importance of cardiac MRI as a diagnostic tool in viral myocarditis-induced cardiomyopathy. Neth Heart J 2009;17:481-486.
Figures
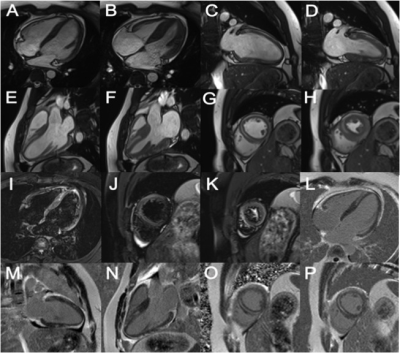
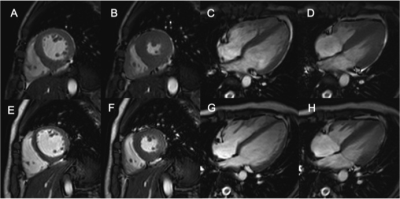
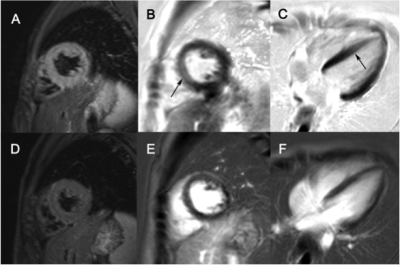
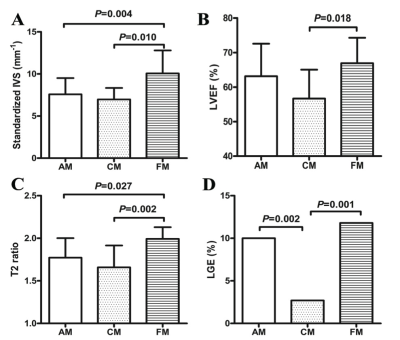
Figure 4 showed the statistical differences of CMR findings between AM, CM and FM children. (A) Standardized IVS, standardized inter-ventricular septal thickness; (B) LVEF, left ventricular ejection fraction; (C) T2 ratio; (D) LGE, late gadolinium enhancement. Compared with AM and CM, higher myocardial thickness and T2 ratio were found in FM children with statistical significance. The LVEF and incidence of LGE in FM children were higher than that in CM children with statistical significance.
CMR, cardiac magnetic resonance; AM, acute myocarditis; CM, chronic myocarditis; FM, fulminant myocarditis.