2779
Synthetic MRI of the Knee: ISMRM/NIST Phantom Validation and In-Vivo Qualitative, Quantitative and Diagnostic Comparison with Conventional MRI of the Diagnosis of Internal Derangement1Radiology, Johns Hopkins Hospital, Baltimore, MD, United States, 2Balgrist University Hospital, Zurich, Switzerland, 3Bond Business School, Gold Coast, Australia, 4Center for Medical Imaging Science and Visualization (CMIV), Linköping University, Linköping, Sweden, 5Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
Knee MRI protocols containing morphologic and quantitative pulse sequences allow comprehensive evaluation of multiple tissues. However, separate quantitative and qualitative image acquisitions are time consuming. We demonstrated excellent native and error-calibrated accuracy of synthetic MRI of the knee for T1, T2 and proton density quantification with use of an ISMRM/NIST phantom, and show excellent intra-day and inter-day repeatability in living human subjects. Synthetic MRI improves contrast-to-noise ratios of cartilage and menisci and yields improvements in artifact reduction and fat suppression. We demonstrate equivalent subjective ratings and diagnostic performance for internal derangement between conventional and synthetic MRI.
Introduction
Quantitative and morphologic MRI is important in assessing knee pain1-3. Synthetic MRI may reduce acquisition times and provide single sequence quantitative and qualitative evaluation.4,5 However, synthetic MRI repeatability and diagnostic performance have not been validated in living subjects for knee evaluation. Error-calibration using a phantom to improve synthetic MRI accuracy has not been demonstrated.Purpose
To test whether synthetic MRI of the knee using an ISMRM/NIST phantom generates accurate and repeatable quantitative T1, T2 and proton density maps, whether error-calibration improves accuracy, and whether synthetic MRI morphologic images are of equal image quality and diagnostic accuracy to conventional MRI.Materials and Methods
Phantom Evaluation
For accuracy validation of the QRAPMASTER sequence, an MRI system phantom was used that was developed by the ISMRM and National Institute of Standards and Technology (NIST)6.
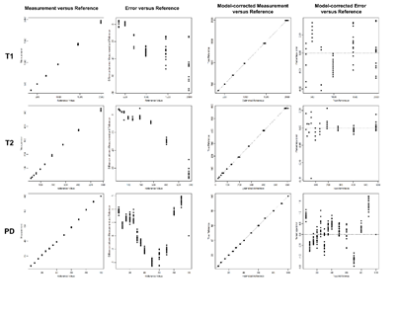
MRI phantom data (Figure 1) was acquired on two consecutive days, two sessions within each day, and twice within each session, in order to assess repeatability. T1, T2 and PD measurements were repeated by a single observer three times with one-week intervals between measurements.
Error calibration equations were derived for T1, T2 and PD layers, after accounting for heteroscedasticity with percentage errors, by using B-spline quadratic curves to match the non-linear structure of the data. Relative errors using reference phantom values were calculated before and after calibration.
Subject Evaluation
Thirty subjects (18 men, 12 women; mean age, 36 years; age range, 18–58 years) underwent the MRI protocol twice on the same day and 10/30 repeated the MRI protocol after 4 (1-9) days.
Quantitative outcomes included intra-day and inter-day agreements of T1, T2 and PD measurements of cartilage on quantitative maps. Measurements were performed in central patellar or trochlear cartilage.
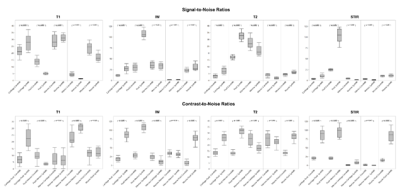
We assessed signal-to-noise (SNR) and contrast-to-noise (CNR) ratios of fluid, cartilage, meniscus, marrow, and muscle on morphological T1, PD, T2, and STIR images of synthetic and conventional MRI. SNR was determined as SI (tissue) / SD (tissue). Contrast-to-noise ratios (CNR) were calculated as |SNR (tissue 1) – SNR (tissue 2)|.
Qualitative outcomes included two observer assessments using a Likert scale of image quality parameters and structural abnormalities. Image quality assessments included overall rating, structure visibility and prevalence of artifacts. Structural abnormalities included integrity of menisci, articular cartilage, anterior cruciate ligament, and subchondral bone.
Statistics
Technique comparisons and repeatability were assessed with the Wilcoxon test for related samples and coefficient of variance (CV), respectively. Cohen’s kappa test was used for agreement analysis. P-values ≤ 0.01 were considered significant.
Results
For phantom evaluation, the average relative error to the reference values was 0.5% (0.1-0.9%) for intra-session measurements, 0.8% (0.6-1.2%) for inter-session measurements, and 1.0% (0.7-1.1%) for inter-day measurements. The average overall relative error was 1.9% (1.0-3.5%), and 0.8% (0.3-1.4%) following error calibration.
T1 fitting with a basic quadratic model yielded the following calibration equation with accuracy of 0.8% (Figure 2):
Reference = =−36.09+√(1302.42+1.59×(Measurement1.95)
T2 fitting with a B-splines quadratic model yielded the following calibration equation with accuracy of 1.4% (Figure 2):
Reference = −43.53+√(1895.19+11.10×(Measurement1.62) if measurement < 195.63,
-935.03+√(1020698+51.72×(Measurement1.62 ) otherwise
PD fitting with a B-splines quadratic model yielded the following calibration equation with accuracy of 0.3% (Figure 2):
Reference = 97.13-√(9433.65-195.82×(Measurement1.01) if measurement < 32.95,
-24.92+√(-1504.66+145.95×(Measurement1.01 ) otherwise,
164.02-√(19994.57-155.14×(Measurement1.01) if measurement > 66.30
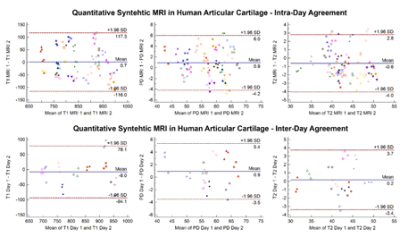
For subject evaluation, intra-day and inter-day comparison of quantitative T1, T2 and PD measurements of articular cartilage showed an average difference of 4.3% and 3.2%, respectively (Figure 2). The intra-day CV was 1.1 for session 1 and 1.2 for session 2. The inter-day CV was 1.3 for both days 1 and 2.
Figure 3 shows tissue SNR and CNR on morphological T1, PD, T2, and STIR images of synthetic and conventional MRI. On PD-weighted, T2-weighted, and STIR images, CNR of synthetic relative to conventional MR were significantly higher between cartilage and fluid and menisci and fluid (p≤0.01 for both).
For structural abnormality assessment (Figure 4), the inter-method agreements were good to very good (reader A kappa = 0.811 (0.692-0.929), reader B kappa = 0.787 (0.662-0.913)). The inter-rater agreements were very good (conventional MRI = 0.858 (0.755-0.96), synthetic MRI = 0.822 (0.704-0.941)).
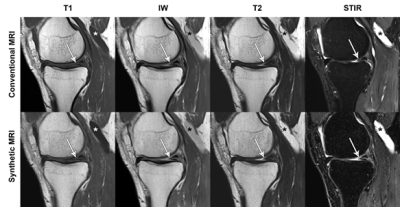
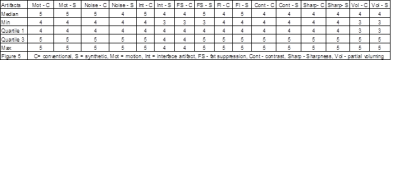
Synthetic MRI improved artifact reduction and fat suppression (p<0.01) (Figure 5). Side-to-side subjective method comparison showed no significant difference (p=0.125).
Conclusion
We demonstrate excellent accuracy of synthetic MRI, which is improved after ISMRM MRI phantom calibration, and at least equal to conventional MRI (7). Synthetic MRI shows excellent repeatability in the knee in living subjects. Synthetic MRI improves morphologic evaluation of cartilage and menisci, artifact reduction and fat suppression. Synthetic MRI on commercially available 3T MRI systems may yield diagnostic and acquisition time advantages.Acknowledgements
No acknowledgement found.References
1. Soellner St, Goldmann A, Muelheims D, Welsch Gh, Pachowsky Ml. Intraoperative Validation Of Quantitative T2 Mapping In Patients With Articular Cartilage Lesions Of The Knee. Osteoarthritis Cartilage. 2017 Aug 8.
2. Anz AW, Lucas EP, Fitzcharles EK, Surowiec RK, Millett PJ, Ho CP. MRI T2 mapping of the asymptomatic supraspinatus tendon by age and imaging plane using clinically relevant subregions. Eur J Radiol. 2014 May;83(5):801-5.
3. Nebelung S, Sondern B, Oehrl S, Tingart M, Rath B, Pufe T, Raith S, Fischer H, Kuhl C, Jahr H, Truhn D. Functional Mr Imaging Mapping Of Human Articular Cartilage Response To Loading. Radiology. 2017 Feb;282(2):464-474. Doi: 10.1148/Radiol.2016160053. Epub 2016 Aug 26.
4. Warntjes JB, Dahlqvist O, Lundberg P. Novel method for rapid, simultaneous T1, T2*, and proton density quantification. Magn Reson Med 2007; 57: 528-37.
5. Hagiwara A, Nakazawa M, Andica C, Tsuruta K, Takano N, Hori M, Suzuki H, Sugano H, Arai H, Aoki S. Dural Enhancement in a Patient with Sturge-Weber Syndrome Revealed by Double Inversion Recovery Contrast Using Synthetic MRI. Magn Reson Med Sci. 2016;15(2):151-2. doi: 10.2463/mrms.ci.2015-0066. Epub 2015 Nov 6.
6. Russek SE, Boss M, Jackson EF, Jennings DL, Evelhoch JL, Gunter JL, Sorensen AG. Characterization of NIST/ISMRM MRI system phantom. In Proceedings of the 20th Annual Meeting of ISMRM, Melbourne, Victoria, Austraia, 2012. Abstract 2456.
7. Bane O, Hectors Sj, Wagner M, Arlinghaus Ll, Aryal Mp, Cao Y, Chenevert Tl, Fennessy F, Huang W, Hylton Nm, Kalpathy-Cramer J, Keenan Ke, Malyarenko Di, Mulkern Rv, Newitt Dc, Russek Se, Stupic Kf, Tudorica A, Wilmes Lj, Yankeelov Te, Yen Yf, Boss Ma, Taouli B. Accuracy, Repeatability, And Interplatform Reproducibility Of T1 Quantification Methods Used For Dce-Mri: Results From A Multicenter Phantom Study. Magn Reson Med. 2017 Sep 14.
Figures