2707
DIXON-type pulse sequence for MRI-only external beam radiotherapy of prostate cancer1Department of Radiation Oncology, National Center for Cancer Care and Research, Hamad Medical Corporation, Doha, Qatar
Synopsis
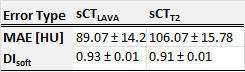
Water-fat separated images provided by the DIXON-type pulse sequence were combined with the multi-scale and dual-contrast patch-based method to generate synthetic-CT (sCT) for MR-only external beam radiotherapy treatment planning of prostate cancer. The benefit of such sequence was demonstrated by retrospective geometric and dosimetric evaluation of sCT on five patients. Compared to reference CT, the mean absolute error was 89.07±14.2HU, the dice coefficient in soft tissues was 0.93±0.01. Good agreement with conventional planning techniques was obtained; the highest percentages of dose metrics deviations were below 0.7% for PTV, 0.05% for the rectum, and 0.01% for the bladder.
INTRODUCTION
The use of MRI sole for external beam radiotherapy planning of patients with prostate cancer require the generation of synthetic-CT(sCT). This task is challenging since MR intensities are not related to the tissues attenuation properties used for dose calculation. T2-weighted MR images were commonly used for sCT generation1.In this study, we investigated the generation of sCT from Dixon-type pulse sequence motivated by its capability to provide water-fat separated images and hence more valuable information for soft-tissues modeling compared to T2w MRI.METHODS
Water-only and Fat-only LAVA-FLEX MRI (W-LAVA, F-LAVA), fat suppressed ‘hybrid’ T2/PD (T2PD) MRI, and CT datasets from 5 patients who underwent prostate radiotherapy were included in this retrospective study. MR images were acquired on GE 1.5T Optima 450w MR scanner whereas CT scans were acquired with a Siemens scanner (Somatom Sensation 16-slice sensation). The data were co-registered and resampled to a matrix size of 256x256x134 voxels and a resolution of 1.4x1.4x1.4mm3. Multi-scale and Dual-contrast Patch-Based Method (MDPBM)2, which was assessed successfully in brain site, was used for generation of two types of sCT: sCTLAVA using W-LAVA and F-LAVA, and sCTT2 using T2PD. For each patient in the database, sCT were generated using Leave-One-Out Cross-Validation.
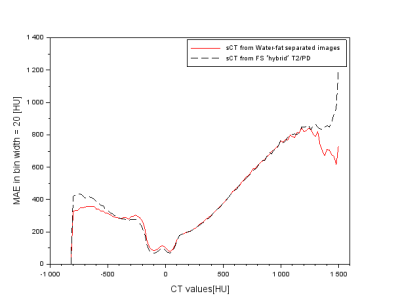
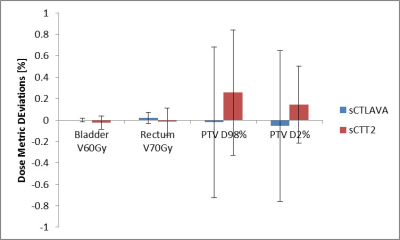
sCTLAVA was benchmarked against sCTT2 visually and quantitatively. The Mean Absolute Error (MAE) between sCT and reference CT was computed for voxels intensities in the pelvis region. The Dice coefficient was calculated for soft-tissues (DIsoft) that were segmented using a threshold range of [-400HU, 200HU]. Furthermore, the range of CT intensities was divided into bins of 20HU for which MAEs were computed. For the dosimetric evaluation, the TPS Eclipse v11.0 (Varian Medical Systems, Paolo Alto, CA) was used. Clinical PTV, the rectum, and the bladder were contoured on MRI and copied to CT and sCT. VMAT plans (6MV, prescribed dose 78.31Gy in 41 fractions, 2Arcs) was generated on sCTLAVA and copied to CT, sCTT2. The dose was calculated by the Analytical Anisotropic Algorithm to account for tissues heterogeneity. Dosimetric assessment was by comparison of the Percentage of Dose Metrics Deviations (PDMD). The percentage of volume receiving 60Gy (V60Gy) and 70Gy (V70Gy) were calculated for the bladder and the rectum respectively. The near maximum (D2%) and the near minimum (D98%) were calculated for the PTV.
RESULTS
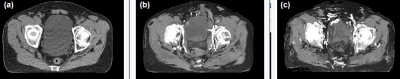
Figure 1 shows a transverse slice in sCTLAVA, sCTT2, and CT for the same location. Table 1 displays the average and standard deviation of MAE and DIsoft for sCTT2 and sCTLAVA. Figure 2 displays the average MAEs in bins of 20HU for sCTLAVA and sCTT2. Figure 3 reports dosimetric errors and standard deviations obtained for OARs and PTV respectively when planning with sCTT2 and sCTLAVA.DISCUSSION
Our results demonstrated significantly better performance of combining water-fat separated images W-LAVA and F-LAVA within MDPBM framework in comparison to T2PD. The absolute dosimetric agreement between sCTLAVA (respectively sCTT2) and CT was below 0.7% (1%) for PTV and 0.05% (0.3%) for OARs. sCTLAVA benefited from better description of soft tissues composition due to the use of water-fat separated images as we hypothesized. Our approach, which is automated and does not require deformable registration, had comparable results to previous techniques reported in the literature 1 .CONCLUSION
We demonstrated that sCT generated from water-fat separated Dixon images could be potentially suitable for MR-only external beam radiotherapy of patients with prostate cancer. Further work will be done to assess and improve the method on more patients.Acknowledgements
No acknowledgement found.References
1. Edmund JM, Nyholm T. A review of substitute CT generation for MRI-only radiation therapy. Radiat. Oncol. [Internet] 2017;12:28. doi: 10.1186/s13014-016-0747-y.
2. Aouadi S, Vasic A, Paloor S, Torfeh T, McGarry M, Petric P, Riyas M, Hammoud R, Al-Hammadi N. Generation of synthetic CT using multi-scale and dual-contrast patches for brain MRI-only external beam radiotherapy. Phys. Medica [Internet] 2017;42:174–184. doi: 10.1016/j.ejmp.2017.09.132.
Figures