2697
A novel method for video-based cardiac gating in 7T MR angiography using a video of the foot1Department of Computer Science, University of Applied Sciences and Arts Dortmund, Dortmund, Germany, 2Erwin L. Hahn Institute for Magnetic Resonance Imaging, University Duisburg-Essen, Essen, Germany, 3Division of Medical Physics in Radiology, German Cancer Research Center, Heidelberg, Germany
Synopsis
In ultra-high-field MRI, cardiac gating is problematic because electrocardiography is prone to magnetohydrodynamic artifacts and pulse oximetry suffers from signal loss during long examinations. The goal of this work is to investigate practical feasibility of cardiac gating based on a video from the sole of the foot that is leaned to a glass plate. We combined this novel setup with an open-source software for video-based cardiac gating (https://github.com/nspi/vbcg) and performed ultra-high-field non-enhanced angiography in one volunteer. As reference, we performed pulse oximetry gating and comparison of maximum intensity projection images shows a similar image quality. Future work will evaluate the feasibility of this novel cardiac gating method in a larger cohort.
Introduction
In many ultra-high-field MRI applications, cardiac gating presents a challenge: electrocardiography (ECG) suffers from magnetohydrodynamic artifacts [1] and pulse oximetry (PO) suffers from signal loss due to poor perfusion because of decreasing patient temperature [2], especially during long examinations. In ultra-high-field non-enhanced angiography (MRA) of the lower extremities, examinations take up to one hour [3]. The lack of a reliable vendor-provided gating method led us in the past to the development of an open-source hardware and software prototype for video-gated MRI [4].
The system utilizes the fact that the cardiac activity can be estimated from subtle skin color variations captured with a video camera [5, 6], a method called photoplethysmography imaging. It allows the measurement of a photoplethysmography signal similar to PO but from a significantly larger area, which could increase robustness to signal loss. In previous work, we used videos from the patients’ forehead and demonstrated the technical feasibility of video-gated MRI, but the poor signal-to-noise ratio (SNR) of the acquired signal posed a challenge [7].
Recently, it has been shown that applying external force to the skin increases the SNR of the cardiac signal [8]. Hence, we developed a novel setup for video acquisition from the sole of the foot in contact with a glass plate. We combined this setup with our open-source system to acquire MRA of the lower extremities of a healthy volunteer (female, 24 years) and compare the results to PO gating.
Methods
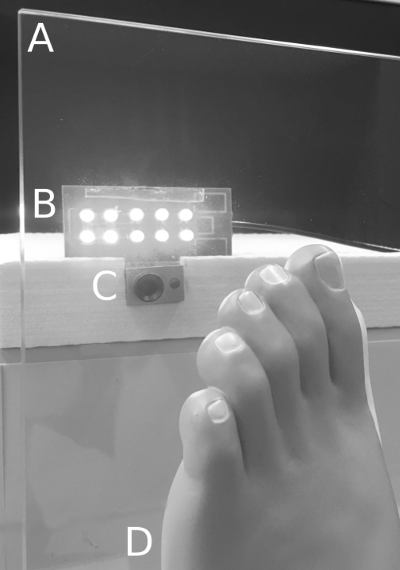
Video acquisition - A schematic visualization of the setup is depicted in Fig. 1: An off-the-shelf glass plate (A; 30x30x0.5 cm) is fixed on the patient table, and the foot (D) is placed against it. The sole is captured by a MR-compatible camera (C; 12M-i, MRC Systems, Heidelberg, Germany; max. 30 frames-per-second (FPS)) placed at a distance of 10 cm and illuminated by a LED array (B; L-7113VGC-E, Kingbright, CA, USA; peak wavelength 518nm). A frame acquired during an MR examination is depicted in Fig. 2.
Video processing - We used our open-source system for video processing and cardiac gating [4]; it processes the camera signal with approximately 25 FPS. A cardiac time signal was acquired by computing the average of all pixel values for each frame. The chosen algorithm [7] automatically finds the largest peak in the signal’s power spectrum within a range of 30-180 beats-per-minute and sends a trigger according to the peak’s phase.
MRA acquisition - Experiments were conducted on an ultra-high-field scanner (Magnetom 7T, Siemens Healthineers, Erlangen, Germany) with the MRA setup proposed by Fischer et al. [2]. The volunteer was positioned feet first on a sliding table. We acquired MRA images at three consecutive table positions, each covering 10cm with an overlap of approximately 2cm. The coil covered the thigh, kneecap, and shank so that different anatomical structures were acquired. For each table position, we first performed image acquisition with PO gating followed by video gating. The vendor-provided PO sensor (50Hz sampling rate) was applied on the index finger of the right hand. During the whole experiment (approx. 30min) repositioning of the foot was not required.
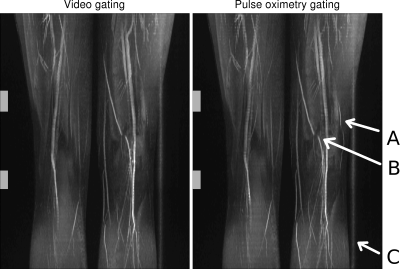
Image processing - Maximum intensity projection (MIP) images in coronal orientation were computed and exported to DICOM format using the MR vendor-provided software. MATLAB 2017 (MathWorks, MA, USA) was used to determine the overlap resulting from different table positions by visual inspection. Subsequently, individual MIP images were blended for both gating modalities.
Results
Blended MIP images are depicted in Fig. 3: Images from both gating modalities show a uniform and intense delineation of the arteries as well as similar contrast. The thigh and kneecap regions acquired via video gating are very homogeneous, whereas in the PO-gated MIP there are more artifacts in the form of short signal declines as a result of inaccurate gating [3]. There is a small vessel that is less clearly visible in the video-gated MIP (A), and there are identical artifacts in both images that are unrelated to gating (B, C).
Discussion and Conclusion
Conventional gating methods in ultra-high-field MRI are prone to either magnetohydrodynamic artifacts (ECG) or signal loss during long examinations (PO). Video-gated MRI could possibly overcome these limitations, and in previous work technically feasibility has been demonstrated [7]. This work investigated the practical feasibility of using a video of the foot for cardiac gating during 7T MRA and image quality is comparable to PO-gating. In future work we aim to evaluate this novel method in a larger cohort.Acknowledgements
No acknowledgement found.References
1. Oster J, Clifford GD. Acquisition of electrocardiogram signals during magnetic resonance imaging. Physiological Measurement 2017;38
2. Hanning CD, Alexander-Williams JM. Pulse oximetry: a practical review. British Medical Journal. 1995;311(7001)
3. Fischer A, Maderwald S, Orzada S, et al. Nonenhanced Magnetic Resonance Angiography of the Lower Extremity Vessels at 7 Tesla. Investigative Radiology 2013;48(7):525-534
4. Spicher N, Orzada S, Maderwald S, Kukuk M, Ladd ME. An open-source hardware and software system for video-gated MRI. Proc. Intl. Soc. Mag. Reson. Med. 25 2017; #141
5. Sun Y, Thakor N. Photoplethysmography Revisited: From Contact to Noncontact, From Point to Imaging. IEEE Transactions on Biomedical Engineering 2015;63(3)
6. Maclaren J, Aksoy M, Bammer R. Contact-free physiological monitoring using a markerless optical system. Magnetic Resonance in Medicine 2015;74(2)
7. Spicher N, Kukuk M, Maderwald S, Ladd ME. Initial evaluation of prospective cardiac triggering using photoplethysmography signals recorded with a video camera compared to pulse oximetry and electrocardiography at 7T MRI. BioMedical Engineering Online 2016;15(1)
8. Kamshilin AA, Nippolainen E, Sidorov IS, et al. A new look at the essence of the imaging photoplethysmography. Scientific Reports 2015; 5(10494)
Figures