2647
Crossed cerebellar diaschisis: diagnostic & prognostic value of BOLD fMRI cerebrovascular reactivity1Neuroradiology, University Hospital Zurich, Zurich, Switzerland, 2Neurosurgery, University Hospital Zurich, Zurich, Switzerland, 3Neurology, University Hospital Zurich, Zurich, Switzerland, 4Nuclear Medicine, University Hospital Zurich, Zurich, Switzerland
Synopsis
Crossed cerebellar diaschisis (CCD) is associated with poorer stroke outcome and is traditionally measured with [15O]-H2O-PET.
BOLD-CVR can detect CCD with high specificity and sensitivity. Furthermore, CCD subjects identified with BOLD-CVR also had a poorer clinical status at baseline and at three months follow-up. These encouraging results suggest that BOLD-CVR might be considered as a diagnostic and prognostic test for CCD subjects, comparable to the gold standard [15O]-H2O-PET – but without the ~1mSv radiation dose.
Introduction
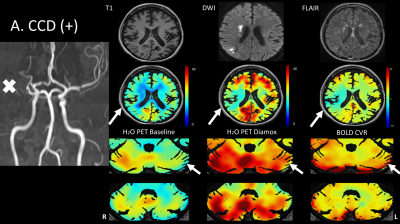
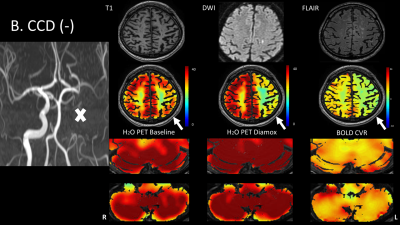
CCD, defined as the reduction in CBF and metabolism contralateral to a supratentorial lesion, corresponds to poorer clinical outcome. Traditionally, PET imaging is used to detect CCD. However, as advanced non-invasive MRI techniques enabling CVR determination are emerging; BOLD derived CVR may be a novel tool to characterize this disease.
Hence, we aimed to study BOLD CVR as a diagnostic and prognostic tool for CCD and comared it to the gold standard [15O]-H2O-PET.
Methods
Nineteen subjects with symptomatic unilateral cerebrovascular steno-occlusive disease (age: 60±13, 7 females) underwent a BOLD functional MRI CVR measurement [1] as well as a [15O]-H2O-PET study. Two subjects underwent the same imaging sequence twice.
CCD as well as a cerebellar asymmetry index were determined from PET and compared to the cerebellar asymmetry index of BOLD CVR quantitative values.
Clinical status at admission and outcome after 3 months were determined with two stroke severity scores (i.e. National Institute of Health Stroke Score and modified Rankin Scale).
Results
Cerebellar asymmetry index in CCD-positive subjects was significantly different for both BOLD CVR and PET (CCD positive vs. CCD-negative for BOLD CVR: 14.76 ± 10.71 vs. 1.40 ± 5.43, p<0.001 and for PET: 7.04 ± 1.75 vs. 1.79 ± 3.14, p<0.001).
The area under the ROC curve for BOLD-CVR was 0.88 (CI: 0.73-1.0) with 0.87 sensitivity and 0.77 specificity to detect CCD.
CCD-positive patients were in poorer clinical condition at baseline (CCD positive vs. CCD negative: National Institute of Health Stroke Score: 6 vs. 1, p = 0.004; modified Rankin Scale: 3 vs. 1, p<0.01) and after 3 months follow-up (National Institute of Health Stroke Score: 2 vs. 0, p=0.03; modified Rankin Scale: 1 vs. 0, p=0.04).
Discussion
BOLD-CVR can detect CCD with high specificity and sensitivity. Furthermore, CCD subjects identified with BOLD-CVR also had a poorer clinical status at baseline and at three months follow-up. These encouraging results suggest that BOLD-CVR might be considered as a diagnostic and prognostic test for CCD subjects, comparable to the gold standard [15O]-H2O-PET – but without the ~1mSv radiation dose.
In a recent feasibility study, Strother et al. [2] demonstrated that CCD subjects identified with ASL (i.e. cerebellar hemispheric CBF asymmetry) also had significantly reduced cerebellar hemispheric BOLD-CVR as compared to control subjects without CBF asymmetry. Significant asymmetric cerebellar hemispheric BOLD signal changes was also shown using a hyperoxic gas challenge in a small cohort with acute large volume MCA strokes. [3]
Using a novel CO2 application technique and improved BOLD-CVR analysis methods [1], we were able to generate high resolution quantitative cerebellar BOLD-CVR maps. With a cut-off point of BOLD-CVR cerebellar asymmetry index of 6.2, CCD was detected with a sensitivity of 0.87 and a specificity of 0.77.
Significance of CCD detection
The incidence of 36.8% CCD-positive subjects in our study is similar to incidences reported by others. Some studies also reported CCD as a prognostic indicator of poorer neurological improvement after cerebral infarction. Our data confirm that CCD is related to worse clinical status at the time of stroke as well as neurological outcome 3 months after stroke.
Oppositely, other studies showed that the presence of CCD in the acute phase has no significant impact on functional outcome. Here, we have to mention that correction of hypoperfusion after acute-stage stroke could shift some subjects from CCD-positive to CCD-negative.
CCD, assessed with PET, at four different time points (before thrombolysis, 3h, 24h and 14 days later) were all strongly correlated with neurological outcome. The subjects that recovered from CCD tended to have a more favorable outcome. Important to mention is that the different methodology between BOLD-CVR and PET imaging may explain the proportional bias seen in the Bland-Altman plot (Figure 4B). In CCD-positive patients, the decrease in cerebellar CBF seems not proportional to the relative metabolism change. Therefore, a proportional bias can be seen when analyzing the entire cohort (Figure 4B). This bias disappears after exclusion of CCD-positive subjects (Figure 4C).
Conclusion
BOLD-CVR can accurately detect CCD in subjects with unilateral steno-occlusive disease. Furthermore, CCD subjects identified with BOLD-CVR had a poorer initial clinical status and outcome after three months for both stroke severity scores. These encouraging findings open to further investigation to better characterize CCD with BOLD-CVR.Abbreviations
ASL: arterial spin labeling,BOLD: blood oxygen-level dependent,
CBF: cerebellar blood flow,
CCD: Crossed cerebellar diaschisis,
CVR: cerebrovascular reactivity,
ICA: internal carotid artery,
MCA: middle cerebral artery,
mRS: modified Rankin Scale,
NIHSS: National Institute of Health Stroke Scale,
PET: Positron Emission Tomography,
Acknowledgements
No acknowledgement found.References
1. van Niftrik CHB, Piccirelli M, et al. Iterative analysis of cerebrovascular reactivity dynamic response by temporal decomposition. Brain and behavior. 2017.
2. Strother MK, et al. CCD after stroke identified noninvasively with CBF-weighted ASL MRI. Eur J Radiol 2016.
3. Dani KA, et al. CCD: insights into oxygen challenge MRI. Journal of cerebral blood flow and metabolism: 2012.
Figures
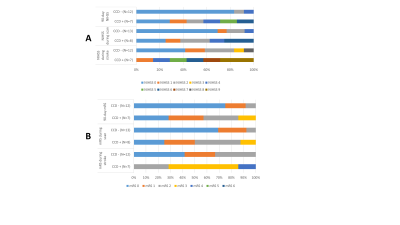
NIHSS scores & mRS scores of CCD-positive and CCD-negative subjects.
National Institute of Health Stroke Scale scores (A) and modified Ranking Scale scores (B) of CCD positive and CCD negative subjects.
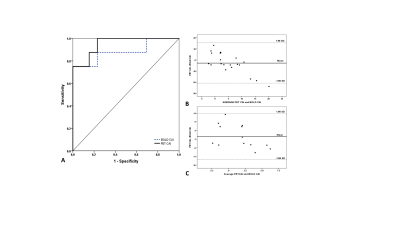
Agreement between PET & BOLD-CVR
Receiver Operating Characteristics Curve (A) of BOLD-CVR and PET for the detection of CCD. Bland Altman plot of the whole cohort (B) and for the CCD negative cohort alone (C). Note that a proportional bias can be seen when considering data of both groups. When considering the CCD negative cohort alone (C), a good agreement is found.