2644
Baseline mrEMVI as an independent prognostic factor for locally advanced rectal cancer with neoadjuvant chemoradiotherapy: recommendations for risk stratification1Radiology, Key laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Radiology, Peking University Cancer Hospital & Institute, BEIJING, China, 2Key laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Radiology, Peking University Cancer Hospital & Institute, BEIJING, China, 3Radiology, Key laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Radiology, Peking University Cancer Hospital & Institute, BEIJING, Christmas Island
Synopsis
Extramural venous invasion status is a potential prognostic factor for identifying rectal cancer patients with a high risk of distant metastasis or local recurrence. It is currently unclear what impact extramural venous invasion status as defined by magnetic resonance imaging before neoadjuvant chemoradiotherapy (pre-NCRT mrEMVI) has on survival outcomes in patients with locally advanced rectal cancer. Moreover, the incorporation of baseline mrEMVI into risk stratification is poorly understood.This study has demonstrated that pre-NCRT mrEMVI status can be reliably evaluated and can serve as an independent prognostic factor for distant and local recurrence and overall survival in patients with locally advanced rectal cancer. We have provided important evidence that pre-NCRT mrEMVI status should be considered for managing risk stratification in baseline locally advanced rectal cancer. Finally, we recommend that mrEMVI evaluation be included in routine pre-NCRT MR reports to support an individualized treatment strategy, considering positive pre-NCRT mrEMVI may serve as an indicator for neoadjuvant chemotherapy.
Purpose
Extramural venous invasion(EMVI) is found exclusively in locally advanced tumors, and has been shown to be associated with higher rates of recurrence and death in rectal tumor. The importance of mrEMVI evaluation has been gradually recognized. However, the role of mrEMVI as an independent prognostic factor remains controversial. There have been no reports on the prognostic impact of pre-NCRT mrEMVI status in rectal cancer patients, and it is still unknown how mrEMVI-defined risk stratification can be used to identify patients with different survival outcomes. This study sought to define the potential role of pre-NCRT mrEMVI status (including location, vascular number and size, and cause of vascular involvement) in predicting the recurrence and survival of patients with locally advanced rectal cancer. In addition, the study aimed to define the risk stratification for locally advanced rectal cancer patients according to pre-NCRT predictors.Methods
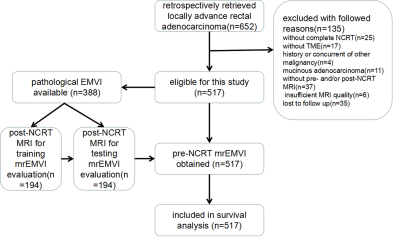
This retrospective study collected patients from the prospective database of Peking University Cancer Hospital for rectal cancer. All patients had locally advanced disease as determined by pre-treatment MRI (T3-4Nx and T1-2N+) and completed neoadjuvant chemoradiotherapy followed by TME.Pre-NCRT and post-NCRT MR images were available for all patients.A total of 517 patients were identified. (Fig 1)An experienced radiologist measured the features on the MRI, including the distance from the inferior part of the tumour to the anal verge (DTA), mesorectal fascia (MRF), tumour stages(mrT stages), lymph node metastasis(mrLN status), tumour location (TL) and tumour involvement in the intestinal lumen (TIL) , on pre-NCRT images of all patients. mrEMVI evaluation was conducted using the 5-score grading system. Firstly, two readers were independently trained for mrEMVI evaluation by using post-NCRT images in half of cases where pEMVI evaluation could be obtained. Secondly, their mrEMVI evaluation were test by using the rest half of cases to make sure their mrEMVI assessments were acceptable (a consistency rate of ≥80% compared with pathology). Thirdly, they independently evaluated pre-NCRT mrEMVI status for all enrolled patients. The number of involved blood vessels(EMVIvasno), the diameter of the involved blood vessel(EMVIdiameter),the location of involved blood vessel(EMVIlocation) and the cause of vascular involvement(EMVIcause) were also measured by two independent readers. Two pathologists independently extract pEMVI status from pathological report. The pEMVI status was recorded as presence, absence and unclear. Finally, we identified 388 patients whose pEMVI status was available, 212 were pEMVI positive, and 176 were pEMVI negative.This analysis aimed to explore the prognostic effect of pre-NCRT mrEMVI evaluation on survival outcomes (as defined by DMFS, LRFS and OS). The chi-square test was used to test the association between mrEMVI status and pre-NCRT MRI features and pathological characteristics. Kaplan-Meier estimates with the univariate log-rank test were used to detect significant prognostic factors and yielded survival curves. The step-wise Cox proportional hazard model was used for multivariate analysis by selecting independent prognostic factors for survival outcomes from all pre-NCRT MRI features and to acquire the adjusted hazard ratios(HR).Results
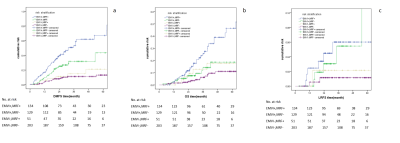
Multivariate Cox analysis showed that pre-NCRT positive mrEMVI and mesorectal fascia(MRF) were independent risk factors for distant metastasis-free survival (DMFS) and overall survival (OS), and mrEMVI(+) was the only independent risk factor for local relapse-free survival (LRFS) (Fig 2). However, pre-NCRT mrEMVI(+) patients who achieved post-NCRT mrEMVI(-) had similar survival to patients who didn’t. EMVI(+)MRF(+) patients had a significantly higher risk of distant metastasis than did EMVI(-)MRF(+) and EMVI(-)MRF(-) patients, and had a significantly higher risk of death than did EMVI(-)MRF(-) patients. (Fig 3). EMVIlocation was the only independent risk factor for DMFS, but it didn’t provide clue for metastasis site.Conclusion
This was a well-designed retrospective study, and eligible cases were consecutively retrieved from a prospective database. This study has demonstrated that pre-NCRT mrEMVI status can be reliably evaluated and can serve as an independent prognostic factor for distant and local recurrence and overall survival in patients with locally advanced rectal cancer. We have provided important evidence that pre-NCRT mrEMVI status should be considered for managing risk stratification in baseline locally advanced rectal cancer. Finally, we recommend that mrEMVI evaluation be included in routine pre-NCRT MR reports to support an individualized treatment strategy, considering positive pre-NCRT mrEMVI may serve as an indicator for neoadjuvant chemotherapy.Acknowledgements
No acknowledgement found.References
1. Kapiteijn E, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 2001; 345:638-646.2. van Gijn W, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 2011; 12: 575-82. 3. Smith NJ, Barbachano Y, Norman AR, Swift RI, Abulafi AM and Brown G. Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. British Journal of Surgery 2008; 95: 229-236. 4. Talbot IC, Ritchie S, Leighton MH, et al. The clinical significance of invasion of veins by rectal cancer. Br J Surg. 1980;67:439-442. 5. Horn A, Dahl O, Morild I. Venous and neural invasion as predictors of recurrence in rectal adenocarcinoma. Dis Colon Rectum. 1991;34:798-804. 6. Michelassi F, Block GE, Vannucci L, et al. A 5- to 21-year follow-up and analysis of 250 patients with rectal adenocarcinoma. Ann Surg.1988;208:379-389. 7. Harrison JC, Dean PJ, el-Zeky F, et al. From Dukes through Jass: pathological prognostic indicators in rectal cancer. Hum Pathol. 1994; 25:498-505. 8. Freedman LS, Macaskill P, Smith AN. Multivariate analysis of prognostic factors for operable rectal cancer. Lancet. 1984; 2:733-736. 9. Mercury Study Group. Diagnostic accuracy of preoperative magnetic resonance imaging in predicting curative resection of rectal cancer: prospective observational study. BMJ 2006; 333: 779.10. Chand M, Evans J,Swift RI, et al. The Prognostic Significance of Postchemoradiotherapy High-resolution MRI and Histopathology Detected Extramural Venous Invasion in Rectal Cancer. Ann Surg 2015; 261(3):473-479.11. Chand M,Swift RI, Tekkis PP, et al. Extramural venous invasion is a potential imaging predictive biomarker of neoadjuvant treatment in rectal cancer. British Journal of Cancer 2014;110: 19–25.12. Pelvic MRI for Guiding Treatment Decisions in Rectal Cancer(http://www.cancernetwork.com) 13. Nougaret S, Reinhold C, Mikhael HW, Rouanet P, Bibeau F, Brown G. The use of MR imaging in treatment planning for patients with rectal carcinoma: have You checked the “DISTANCE”? Radiology 2013; 268(2): 330-344.14. Wang L, Li ZY, Li ZW, et al. Efficacy and safety of neoadjuvant intensity-modulated radiotherapy with concurrent capecitabine for locally advanced rectal cancer. Dis Colon Rectum 2015; 58(2):186-192.15. But-Hadzic J, Anderluh F, Brecelj E, et al. Acute Toxicity and tumour Response in Locally Advanced Rectal Cancer After Preoperative Chemoradiation Therapy With Shortening of the Overall Treatment Time Using Intensity-Modulated Radiation Therapy With Simultaneous Integrated Boost: A Phase 2 Trial. Int J Radiat Oncol Biol Phys. 2016; 96(5):1003-1010.16. Wittekind C, Meyer HJ: TNM Classification of Malignant Tumours 2010 ed 7 Weinheim, Germany Wiley.17. Sohn B, Lim JS, Kim H,, et al. MRI-detected extramural vascular invasion is an independent prognostic factor for synchronous metastasis in patients with rectal cancer. Eur Radiol 2015; 25:1347-1355.18. Bugg WG, Andreou AK, Biswas D. The prognostic significance of MRI-detectedextramural venous invasion in rectal carcinoma. Clinical Radiology 2014; 619:e623.Figures