2628
Comparison of MRI and CT Characterizations of Lung Lesions from Pulmonary Tuberculosis1Radiology, The People's Hospital of Longhua, Shenzhen, China, 2Radiology and Imaging Sciences, Emory University School of Medicine, Atlanta, GA, United States, 3Radiology, Cancer Hospital Chinese Academy of Medical Science, Shenzhen Center, Shenzhen, China
Synopsis
Lung MRI can be applied to imaging and characterize the abnormalities and lesions in patients with history of pulmonary tuberculosis (TB). By comparing with the images obtained from the routine clinical CT from the same patients, this work shows that MRI is comparable to CT as a non-radiation alternative for lung imaging with good diagnostic image quality. In addition, MRI can provide additional information on lung soft tissue properties not available from CT.
Introduction
Given ionizing radiation involved in CT, there is an increased concern on repeated use of CT in patients with tuberculosis (TB), non-cystic fibrosis1, pneumonia2, and lung cancer who need follow-up observations. Cautions are also given when using CT for pregnant women3, children and adolescents. MRI not only can be used as a potential non-radiation imaging alternative to CT for radiological examination of lung, but also can provide additional information on the change of soft tissue properties that is not available from CT. However, due to the technical challenges in low signal and susceptibility artifacts as well as inherited difficulty in motion control, so far, there are limited reports and clinical experiences in use of MRI for the diagnosis and characterization of abnormalities from pulmonary tuberculosis4. In this study, we compared the MRI characterizations of lesions from various cases of obsolete pulmonary tuberculosis with the images from patients’ routine clinical CT to investigate the performance of MRI and its potential clinical implementation.
Materials and Methods
Participants: Twenty-nine patients with history of pulmonary tuberculosis (20 males, 9 females, mean age of 46 years old) who had clinical routine CT scans were recruited in this study. All patients were diagnosed TB by the routine clinical examinations for tuberculosis, including chest CT, and had been treated for TB. Written consents were obtained from all participants. Subjects were screened for MRI safety before MRI scan. MRI and CT scans: All MRI scans were performed with subject free breathing on a 1.5 T MR scanner (Siemens Avanto) using a 12-element body wrap coil. Images were recorded using a chest MRI protocol built and optimized for imaging lung, including T1-vibe-dixon, T2-weighted turbo spin echo (TSE) and T2-weighted TSE fat suppressed imaging sequences with imaging parameters of: FOV=360 mm, matrix of 256x256, TR/TE=3000/60 ms for axial imaging and TR/TE=5000/100 ms for coronal imaging, FA=150 degree. 46 slices with 3 mm slice thickness with no gap was used to cover the lung (resolution: 1.1x1.1x3 mm3). To minimize the respiratory motion artifacts, T2-weighted and T2-weighted fat suppressed coronal images were recorded with parameters of TR/TE=4000/85 ms and 3000/85 ms using a liver dome scout combine with BLADE technique for suppressing motions. CT (GE Optima) images were obtained using parameters: KV=120, mAs=240, slice thickness=5 mm and matrix of 512x512 with window level/wide=-600/1500. Data Analysis All images from CT and MRI of each patient were evaluated by two experienced radiologists double-blinded. The location, size and type of the lesion found in MRI and CT are compared. Paired statistical analysis was used to correlate the findings from CT and MRI.
Results and Discussions
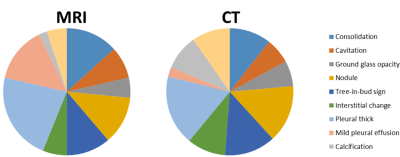
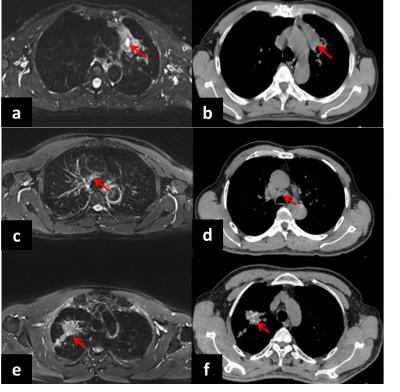
MRI was able to readily detect various lung abnormalities, including: 1) pulmonary nodules (n=12), 2) pulmonary consolidation (n=4), 3) pulmonary bulla (n=2), 4) ground-glass opacity (GGO) (n=5), 5) tree-in-bud sign (n=7), and 6) lung interstitial involvement (n=3). All lesions found in MRI scans of the selected patients were also found in the CT images of those patients (Figure 1). MRI is comparable to CT when identifying most of abnormal features of the lesions, such as nodule, consolidation, cavitation and tree-in-bud sign (Figure 1). However, MRI is less effective in detecting some abnormalities, such as calcification and interstitial change. With high resolution (e.g., 3 mm slice thickness) and soft tissue contrast, MRI showed sufficient sensitivity to the small pulmonary nodules (diameter ≤ 5mm) (n=8), comparing the routine clinical CT. Particularly, MRI is more sensitive and specific to detect pleural or lymph nodes involvement, especially slight pleural effusion (n=9) as shown in Figure 2 or caseous necrosis of lymph nodes (n=1) using fat-suppressed T2 weighted imaging (Figure 3), while CT was less effective and sensitive even at higher spatial resolution. In comparison, CT has advantages for detecting micro-nodules with higher sensitivity and calcification (n=19) with higher specificity (Figure 3). Overall, lung MRI provided interpretable diagnostic images for abnormalities in the lung with manageable respiratory and motion artifacts.
Conclusions
While routine clinical CT provides high resolution images of lung, MRI was able to provide motion reduced high resolution images of lungs and identify various types of lesions of pulmonary tuberculosis and others with less concern of radiation. Each modality exhibits its strength and weakness in identifying specific types of lesions. Nevertheless, the current study suggests that clinical implementation of MRI for imaging pulmonary tuberculosis is feasible and potentially offers more diagnostic information than the clinical standard CT.
Acknowledgements
No acknowledgement found.References
1. Montella, S., et al., Magnetic resonance imaging is an accurate and reliable method to evaluate non-cystic fibrosis paediatric lung disease. Respirology, 2012. 17(1): p. 87-91.
2. Montella, S., et al., Assessment of chest high-field magnetic resonance imaging in children and young adults with noncystic 쳒brosis chronic lung disease: comparison to high-resolution computed tomography and correlation with pulmonary function. Investigative radiology, 2009. 44(9): p. 532-538.
3. Schloß, M., et al., Magnetic Resonance Imaging of the Lung as an Alternative for a Pregnant Woman with Pulmonary Tuberculosis. Journal of radiology case reports, 2015. 9(5): p. 7.
4. Rizzi, E.B., et al., Detection of Pulmonary tuberculosis: comparing MR imaging with HRCT. BMC Infect Dis, 2011. 11: p. 243.
Figures