2576
In-bore MR guided prostate biopsy using multiparametric MRI to avoid unnecessary biopsies1Department of NMR and MRI Facility, All India Institute of Medical Sciences, New Delhi, India, 2Department of Radiology, All India Institute of Medical Sciences, New Delhi, India, 3Department of Radiology, IRCH, All India Institute of Medical Sciences, New Delhi, India, 4Philips Health Systems, Philips India Ltd., Gurgaon, India, 5Department of Pathology, All India Institute of Medical Sciences, New Delhi, India, 6Department of Urology, All India Institute of Medical Sciences, New Delhi, India
Synopsis
We report the results of the pilot study carried out using multiparametric (mp) MRI and in-bore MRI-guided prostate biopsy for detection of PCa to reduce the number of unnecessary biopsies. 11 patients were recruited based on prostate specific antigen > 4ng/ml and abnormal digital rectal examination. In-bore MRI targeted lesions with high PIRADS scores (3 to 5) were correlated with the histopathological findings. The average ADC in PCa patients was significantly lower than the prostatitis and BPH patients. Out of 11 patients, 3 showed adenocarcinoma, 5 prostatitis and 3 BPH.
Purpose:
To target accurately suspicious areas of malignancy for MR guided in-bore biopsy method using multiparametric (mp) MRI approach for diagnosis of prostate cancer (PCa).
Introduction:
PCa is the second most common cancer worldwide and increasing incidence rate every year. Digital rectal examination (DRE) and serum prostate specific antigen (PSA) are used for screening of patients suspected to have prostate cancer. The aim of this study is to carry out MR guided in-bore biopsy using mpMRI approach to localize suspicious areas of malignancy in prostate and to reduce unnecessary biopsies.
Methods:
Patients were recruited based on PSA > 4 ng/ml and abnormal DRE. MRI investigations were carried out at 3.0 T MRI system (Achieva, Philips, Netherlands) using a combination of SENSE Flex large and small coils. A mp-MRI approach that consists of T1WI, T2WI, DWI and DCE-MRI was carried out on 11 patients (age = 52 – 70 years; PSA range 4 to 65ng/ml). The T2W images were acquired with the following parameters: repetition time (TR) 6100 ms, echo time (TE) 100 ms, field of view = 240 x 240 mm, and slice thickness of 3 mm. Diffusion weighted images were acquired using seven b-values 0, 200, 400, 800, 1000, 1500 and 2000 s/mm2. ADC values of tumor regions were calculated from ADC map. For DCE-MRI, 20 ml Gadodiamide was injected with saline flush at a rate of 3ml/s. T1W images are obtained every 2-4 s through the prostate. In-bore biopsy was performed on the suspicious area of malignancy directly in the bore of the magnet using a DynaTrim (Invivo, USA) biopsy device with needle guide and DynaCad software. Biopsy was carried out by transrectal approach and localization of lesion was confirmed using MR imaging before the targeted biopsy. Three to six cores were collected from the suspicious areas using 18G needle. All lesions were assigned a score based on PI-RADS classification system1. Institute ethics committee approved the study and informed consent was taken from all subjects.
Results:
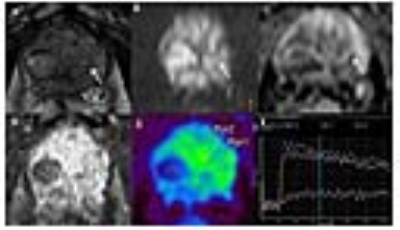
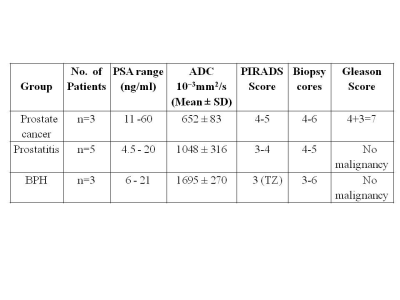
Our data demonstrated that use of mpMRI enables biopsy to be targeted accurately on suspicious area that helps in PCa diagnosis (Figure 1). These MRI targeted lesions with high PIRADS scores (3 to 5) were correlated with the histopathological findings. ADC values of same regions of tumor were also calculated from ADC map. The average ADC in PCa patients was significantly lower than in prostatitis and BPH patients (Table 1). Histopathological findings of all patients who underwent MRI guided biopsy showed PCa and BPH along with features of chronic prostatitis. Prostatitis and BPH have altered cellular density and bacterial infection in interstitial space of tissues. In our study we observed that the MR characteristics on T2W and DWI mimic cancer in many patients with prostatitis. Out of 11 patients, 3 showed adenocarcinoma, 5 prostatitis and 3 BPH with benign metastatic glands stroma and fibromuscular tissue free of tumor.
Discussion:
This study presents the preliminary result of in-bore MRI-guided prostate biopsy using mpMRI approach for detection of PCa. Our data indicated that this approach reduces the number of unnecessary biopsies. Method showed that accurate targeting of the lesion of the suspicious area for biopsy is possible with the use of mpMRI. This procedure improves the diagnostic accuracy of PCa; however, further studies on more number of patients are required.
Conclusion:
Our pilot study suggests that mpMRI followed by in bore MR-targeted biopsy may help accurate targeting the suspicious lesion for biopsy and reduce the sampling error.
Acknowledgements
No acknowledgement found.References
1. PI-RADS™ v2 Prostate Imaging – Reporting and Data System, ACR, Radiology, 2015 version.Figures