2559
Comparison of Prostate Volume Measured by Transrectal Ultrasonography and Magnetic Resonance Imaging with the Actual Prostate Volume Measured after Radical Prostatectomy1Radiology, Chung-Ang University Hospital, Seoul, Republic of Korea, 2Diagnostic Radiology, MD Anderson Cancer Center, Houston, TX, United States
Synopsis
A determination of prostate gland volume facilitates an assessment of prostate disorders and, for prostate cancer, in conjunction with other parameters, can help predict the pathologic stage of disease, offer insights into the prognosis, and help predict treatment response Prostate volume can also be used for calculating prostate-specific antigen density (PSAD) when selecting active surveillance candidates.
The measuring the volume of prostate removed by radical prostatectomy as performed in the present study may be an appropriate way to assess the actual prostate volume even though it may be cancerous. The present study aimed to compare the prostate volume, as measured by TRUS and by MRI, with that of the actual prostate volume measured after a radical prostatectomy.
INTRODUCTION: Prostate volume estimates may be useful for radical prostatectomy, brachytherapy, and benign prostate surgery planning1-7. Prostate volume can also be used for calculating prostate-specific antigen density (PSAD) when selecting active surveillance candidates3, 4–6. More recently, the accuracy of prostate volume calculation has taken on greater importance with the increased popularity of active surveillance4. An increasing number of patients are receiving both transrectal ultrasonography (TRUS) and magnetic resonance imaging (MRI) and may have prostate volume estimates that are discordant between these two methods. In these situations, the imaging modality that provides the most accurate volume is unknown3.
Certainly, the best way to assess the accuracy of a clinically applied method to measure prostate volumes would be to compare the results with the actual prostate volume. Therefore, measuring the volume of prostate removed by radical prostatectomy as performed in the present study may be an appropriate way to assess the actual prostate volume even though it may be cancerous1. The present study aimed to compare the prostate volume, as measured by TRUS and by MRI, with that of the actual prostate volume measured after a radical prostatectomy.
METHODS: This retrospective study included 80 patients who had undergone a radical prostatectomy. TRUS prostate volumes were calculated using the prolate ellipsoid volume formula, with the anteroposterior diameter measured from axial (TRUS-V). Two prolate ellipsoid volumes with the anteroposterior diameter measured from axial (MRI-V1) and mid-sagittal images (MRI-V2) were calculated from the MRI using the same method, and semi-automatically computed volume (MRI-SAV). The actual prostate volume (Actual-V) from specimen weight was measured after a radical prostatectomy. We then divided the measured total prostate weight by 1.05 g/ mL (density of prostatic tissue) and used the resulting volume estimate as the reference standard.
RESULTS: Mean of Actual-V was 38.7ml (20.95–101.9). In paired sample tests, the correlation coefficients (R) for all methods were over 0.9. The best estimate of prostate volume was obtained with MRI-V2 (R = 0.9625). In a student’s t test (paired), TRUS-V (p < 0.0001) showed significant difference compared to the Actual-V. On the other hand, MRI-V2 (p = 0.6819), MRI-V1 (p = 0.3794) and MRI-SAV (p = 0.2956) showed no significant differences.
DISCUSSION: Total prostate weight was obtained from pathology reports. A strong correlation between prostate weight and displaced water volume (R=0.997) was reported previously7, 9.
There may be volume changes that occur in vivo in MR imaging with an endorectal coil; however, there are also potential volume changes in the ex vivo specimens that occur prior to weight measurement6. Direct measurement of the prostate volume can be performed on radical prostatectomy specimens. However, this method does not necessarily determine the true in vivo prostate volume due to shrinkage caused by the loss of blood supply2, 8. The volume might also be overestimated due to adjacent periprostatic tissue2.
CONCLUSION: In this study, MRI and TRUS gave different volumes. MRI is more accurate than TRUS for determining the prostate volume. Furthermore, prolate ellipsoid volumes with MRI is simple, almost as accurate as semi-automatically computed volume with MRI, they should be the preferred method for measuring the prostate volume.
Acknowledgements
No acknowledgements found.References
1. Jeong CW, Park HK, Hong SK, et al. Comparison of prostate volume measured by transrectal ultrasonography and MRI with the actual prostate volume measured after radical prostatectomy. Urol Int 2008; 81(2):179-185
2. Lee JS, Chung BH. Transrectal ultrasound versus magnetic resonance imaging in the estimation of prostate volume as compared with radical prostatectomy specimens. Urol Int 2007; 78(4):323-327
3. Paterson NR, Lavallée LT, Nguyen LN, et al. Prostate volume estimations using magnetic resonance imaging and transrectal ultrasound compared to radical prostatectomy specimens. Can Urol Assoc J 2016; 10:264-268
4. Weiss BE, Wein AJ, Malkowicz SB, Guzzo TJ. Comparison of prostate volume measured by transrectal ultrasound and magnetic resonance imaging: is transrectal ultrasound suitable to determine which patients should undergo active surveillance? Urologic Oncology 2013; 31: 1436–1440
5. Dianat SS, Rancier Ruiz RM, Bonekamp D, Carter HB, Macura KJ. Prostate volumetric assessment by magnetic resonance imaging and transrectal ultrasound: impact of variation in calculated prostate-specific antigen density on patient eligibility for active surveillance program. J Comput Assist Tomogra 2013; 37: 589–595
6. Bulman JC, Toth R, Patel AD, et al. Automated computer-derived prostate volumes from MR imaging data: comparison with radiologist-derived MR imaging and pathologic specimen volumes. Radiology 2012; 262: 144–151
7. Karademir l, Shen D, Peng Y, et al. Prostate volumes derived from MRI and volume-adjusted serum prostate-specific antigen: correlation with Gleason score of prostate cancer. AJR Am J Roentgenol 2013; 201(5): 1041–1048 8. Lukacs S, Vale J, Mazaris E. Difference between actual vs. pathology prostate weight in TURP and radical robotic-assisted prostatectomy specimen. Int Braz J Urol 2014; 40(6):823-827
9. Varma M1, Morgan JM. The weight of the prostate gland is an excellent surrogate for gland volume. Histopathology. 2010; 57(1):55-58.
Figures
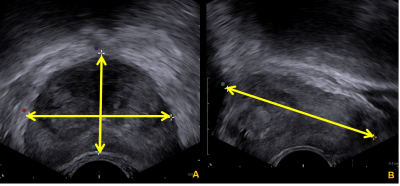
Figure 1. A-61-year old man with measurement of prostate volume by TRUS.
(A) AP diameter (height) and transverse diameter (width) are measured by axial scan.
(B) Longitudinal diameter (length) is measured by mid-sagittal scan.
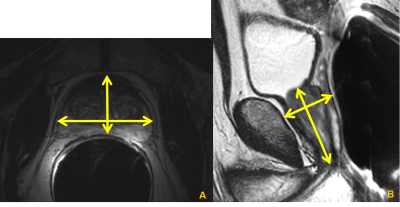
Figure 2. A-61-year old man with measurement of prostate volume by MRI.
(A) AP diameter (height) and transverse diameter (width) are measured by axial scan.
(B) Longitudinal diameter (length) and AP diameter (height) are measured by mid-sagittal scan.
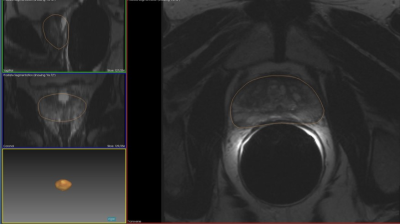
Figure 3. A-61-year old man with semi-automated computer-derived prostate volume by MRI.
Manual drawing of the prostatic tissue boundary and automatically generated 3D image of the prostate.
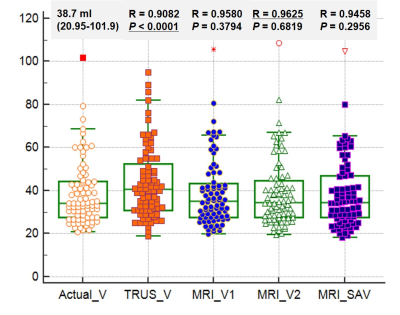
This graph shows comparison between actual prostate volumes by radical prostatectomy and measured prostate volumes by TRUS and MRI. The correlation coefficients (R) for all methods were over 0.9. The best estimate of prostate volume was obtained with MRI-V2 (R = 0.9625). Height (AP diameter) was measured on sagittal scan of MRI.
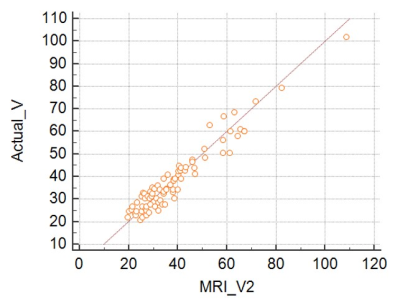
This graph shows comparison between actual prostate volumes by radical prostatectomy and measured prostate volumes by MRI. Height (AP diameter) was measured on sagittal scan of MRI. The best estimate of prostate volume was obtained with MRI-V2 (R = 0.9625).
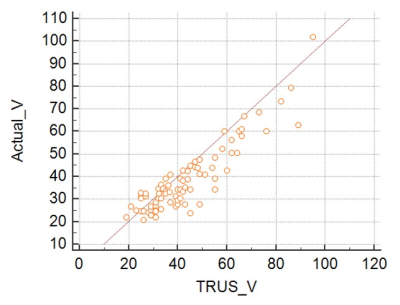
This graph shows comparison between actual prostate volumes by radical prostatectomy and measured prostate volumes by TRUS. In a Student’s t test (paired), the correlation coefficient (R) was over 0.9. However, TRUS-V showed significant difference compared to the Actual-V (p < 0.0001) .