2558
Image quality of WB-MRI in staging recurrent prostate cancer: a multicentre, multinational, multivendor, multiscanner study.1Centre for Medical Imaging, University College London, London, United Kingdom, 2London Health Sciences Centre, London, ON, Canada, 3Royal Marsden Hospital, Sutton, United Kingdom, 4Monash, Melbourne, Australia, 5Peter McCallum Cancer Centre, Melbourne, Australia, 6University of Toronto, Toronto, ON, Canada, 7Laval Quebec, Quebec, QC, Canada, 8Olivia Newton-John Cancer Centre, Melbourne, Australia, 9St Vincents Cancer Center, Sidney, Australia
Synopsis
Whilst whole body (WB) MRI offers substantial promise in cancer staging, considerations regarding image quality are lacking in the literature, yet are essential for the effective delivery of the technique. Here we report the image quality of WB-MRI in 86 patients with suspected biochemical recurrence in prostate cancer in a trial carried out over 3 continents (Australia, America and Europe). We show that the image quality of WB-MRI varies substantially between anatomical sites and centres, particularly for diffusion-weighted sequences, which emphasizes the need to optimise sequences carefully prior to establishing a WB-MRI practice.
INTRODUCTION
Whole body (WB) MRI has changed the patient management pathway in multiple myeloma1 and holds promise in other tumour types such as breast cancer2, lymphoma3 and prostate cancer4. However, literature concerning image quality in whole body WB-MRI is lacking, which is critical to its delivery as an effective staging tool. The aim of the present study is to evaluate image quality in patients with suspected biochemical recurrence in prostate cancer as part of a multicentre, multinational study carried out over 3 continents (Australia, North America and Europe).METHODS
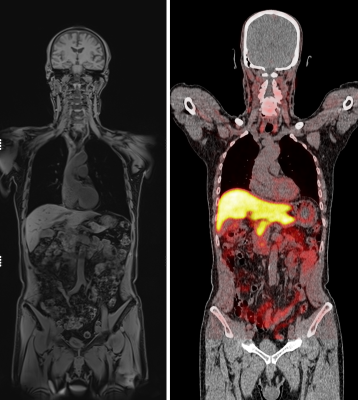
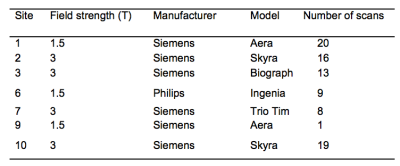
86 men with a median age of 65.2 (IQR 56.6 – 71.1) were consecutively selected. All patients underwent mDixon or T1W and axial DWI at 1.5 or 3 Tesla (T) using gradients of b=50 and 1000 s/mm2. Coverage was from skull base to mid thighs for both sequences. Typical images are provided in figure 1, compared with choline PET/CT. Details of MR scanners are provided in figure 2.
WB-MRI review
A board certified radiologist (SP with 12 years experience) reviewed anonymised MR datasets using Osirix workstations (Pixmeo, Bernex, Switzerland), blinded to all clinical and imaging results. Overall image quality was scored for each imaged region (head, neck, thorax, abdomen, pelvis, thigh) using a 1 – 5 ordinal scale modified from 5–7 (1= uninterpretable, non-diagnostic 2 = poor, non-diagnostic, 3= acceptable for diagnosis, 4 = good, 5 = excellent) for both T1WI and DWI sequences.
Statistical methods
Data were analysed using SPSS Statistics version 23 (2015, IBM, NY, USA) and GraphPad Prism version 6 (2014, San Jolla, CA, USA).
Statistical significance was set at p<0.05 and data were checked for normality using the Shapiro-Wilk test.
The following statistics were used to assess image quality in all patients (n=86):
· Comparison of the mean overall image quality of all anatomical regions for T1WI vs. DWI using Wilcoxon matched pairs testing.
· Comparison of overall image quality of each anatomical region for T1WI and DWI using Friedman’s test with Dunn’s multiple comparison correction.
· Comparison of T1WI and DWI sequences across different sites using Kruskal-Wallis testing and Dunn’s multiple comparisons correction.
RESULTS
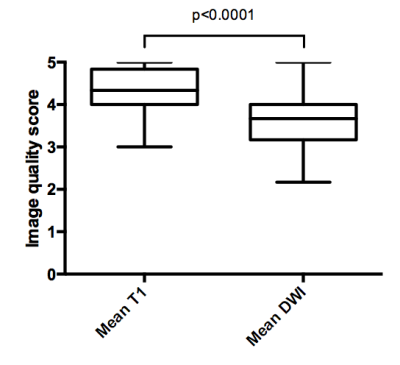
A comparison of T1 and DWI image quality for the mean of all anatomical regions is shown in figure 3, with the results of the Wilcoxon matched pairs test also indicated. The mean score of T1W sequences was 4.28 (SD: 0.50) vs. 3.58 (SD: 0.37) for DWI.
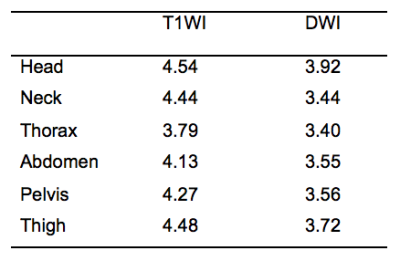
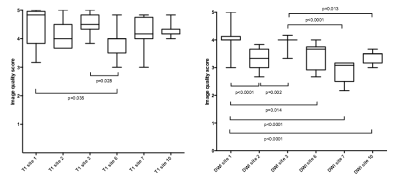
The mean image quality of each anatomical region for both T1 and DWI is shown in figure 4.
Friedman’s testing showed the thorax had significantly lower image quality than the head (p<0.0001), neck (p<0.0001), abdomen (p=0.009), pelvis (p=0.0001) and thigh (p<0.0001), with the abdomen vs. thigh also achieving statistical significance (p=0.02). For DWI, the head had statistically higher values than the neck (p=0.005), thorax (p<0.0001), abdomen (p=0.01) and pelvis (p=0.03). The thorax and thigh also reached statistical significance than the thigh (p=0.01).
The mean image quality of T1WI and DWI sequences across centres are shown in figure 5, with significant differences following Kruskal-Wallis testing with Dunn’s multiple comparison correction indicated.
DISCUSSION
Whilst PET/CT has been recommended for use as a staging modality in cases of biochemical recurrence with a PSA >1ng/ml8, its use is limited by availability, cost and ionizing radiation exposure and has low sensitivity at lower PSA levels. Whilst WB-MRI offers a potential solution to such problems, issues surrounding image quality need to be elucidated.
Image quality in multicentre studies is important since suboptimal scanning protocols may compromise diagnostic performance. The observation that the overall image quality of T1WI sequences was significantly higher than DWI is perhaps unsurprising since the latter are acquired using EPI acquisitions, which are more prone to artefacts such as distortion and ghosting. We also found that image quality can differ significantly between centres for both sequences, and were again more pronounced for diffusion sequences. This emphasizes the importance of effective protocol optimisation in WB-MRI practice whereby the number technical false errors due to suboptimal image quality can be reduced. The finding that image quality varies between stations, and is specifically lower in the thorax vs. the head, which is likely to be due to lower SNR and movement artefact associated with cardiac motion, chest wall and diaphragmatic excursion. Poorer image quality in the neck and shoulder stations is consistently found with diffusion-weighted sequences9,10. Such findings are important targets for sequence development and should also be considered when constructing reports, as images are commonly compromised in these regions.
CONCLUSION
The image quality of WB-MRI varies substantially between anatomical sites and centres, particularly for diffusion-weighted sequences, which emphasizes the need to optimise sequences carefully prior to establishing a WB-MRI practice.Acknowledgements
This project is sponsored by funds from the Movember charity.
References
1. Messiou C, Kaiser M. Whole body diffusion weighted MRI – a new view of myeloma. 2015; : 29–37.
2. Pearce T, Philip S, Brown J, Koh DM, Burn PR. Bone metastases from prostate, breast and multiple myeloma: Differences in lesion conspicuity at short-tau inversion recovery and diffusion-weighted MRI. Br J Radiol 2012; 85: 1102–6.
3. Punwani S, Taylor S a., Saad ZZ, et al. Diffusion-weighted MRI of lymphoma: Prognostic utility and implications for PET/MRI? Eur J Nucl Med Mol Imaging 2013; 40: 373–85.
4. Lecouvet FE, El Mouedden J, Collette L, et al. Can whole-body magnetic resonance imaging with diffusion-weighted imaging replace tc 99m bone scanning and computed tomography for single-step detection of metastases in patients with high-risk prostate cancer? Eur Urol 2012; 62: 68–75.
5. Barth BK, Cornelius A, Nanz D, Eberli D, Donati OF. Comparison of image quality and patient discomfort in prostate MRI: pelvic phased array coil vs. endorectal coil. Abdom Radiol 2016; 41: 1–9.
6. Heijmink SWTPJ, Fütterer JJ, Hambrock T, et al. Prostate cancer: body-array versus endorectal coil MR imaging at 3 T--comparison of image quality, localization, and staging performance. Radiology 2007; 244: 184–95.
7. Hausmann D, Bittencourt LK, Attenberger UI, et al. Diagnostic accuracy of 18F choline PET/CT using time-of-flight reconstruction algorithm in prostate cancer patients with biochemical recurrence. Clin Nucl Med 2014; 39: e197–201.
8. Heidenreich a, Bolla M, Joniau S, et al. Guidelines on Prostate Cancer. Update 2011; 53: 31–45.
9. Attariwala R, Picker W. Whole body MRI: Improved lesion detection and characterization with diffusion weighted techniques. J Magn Reson Imaging 2013; 38: 253–68.
10. Eiber M, Holzapfel K, Ganter C, et al. Whole-body MRI including diffusion-weighted imaging (DWI) for patients with recurring prostate cancer: Technical feasibility and assessment of lesion conspicuity in DWI. J Magn Reson Imaging 2011; 33: 1160–70.