2529
Optical unobtrusive physiology sensor for respiratory-triggered MRI acquisitions1Philips Research, Hamburg, Germany, 2Philips Research, Eindhoven, Netherlands, 3Philips Healthcare, Bothell, WA, United States, 4Philips Innovation Services, Eindhoven, Netherlands
Synopsis
A prototype in-bore camera-based physiology sensor was developed and applied for respiratory-triggered MR acquisitions on volunteers. The camera-based physiology sensor allows unobtrusive measurement of breathing activity by derivation of respiratory signals from video stream in real-time. The camera-based breathing sensor provided high quality breathing signal reliably under all tested circumstances of a volunteer study. The breathing signal quality was rated to be superior compared to the bellows in terms of SNR and signal characteristics. Potential false triggers where significantly reduced by the camera. The resulting image quality was on average superior when triggering off the camera compared to when triggering off the bellows.
Purpose
A prototype in-bore camera-based physiology sensor was developed and applied for respiratory-triggered MR acquisitions on volunteers. The camera-based physiology sensor allows unobtrusive measurement of breathing activity by derivation of respiratory signals from video stream in real-time. Focus of the investigation was the comparison of the camera sensor to the standard bellows sensor with respect to resulting respiratory signal and MR image quality in respiratory-triggered MRI acquisitions performed in volunteers.
Methods
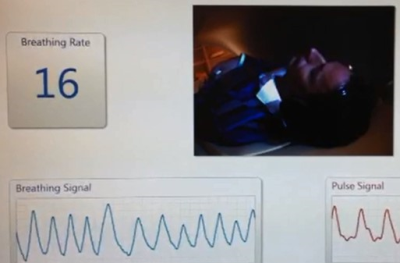
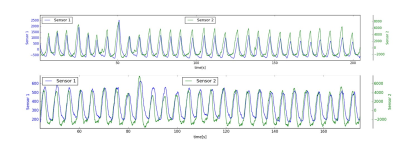
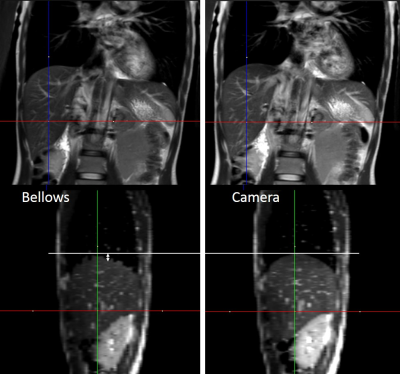
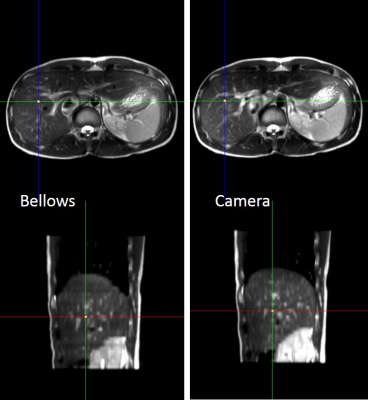
An RGB camera with infrared cut filter of type IDS uEye (IDS Imaging, Obersulm, Germany) was used to acquire in-bore videos during MR image acquisition. The camera was attached on the cover of a 3T Ingenia MRI scanner (Philips Healthcare, Best, Netherlands) at the rear flare of the magnet Fig.1. The used camera position allowed a favorable viewing angle so that the upper body could be monitored while subject obstruction by accessories, coils, pillows/blankets or bodyparts as well as collisions could be avoided. The bore-lights at the back-end of the scanner were used for in-bore illumination (Fig.2). The camera was shielded in a copper housing and the USB-PC connection cable was equipped with 3 cable traps (baluns) tuned for 3T (Fig.1). Breathing signals were derived in real-time from the camera video stream using the algorithm described in [1]. The camera sensor server was connected to the MR system network and the signals were streamed to the data acquisition system so that they could be used equivalently to a standard respiratory bellows sensor for respiratory-triggered MRI acquisitions. Comparable camera setups have been described earlier [2,3]. Signals from the respiratory bellows and the camera were available simultaneously and could be stored into a physiology log-file for signal comparison. 17 Volunteers underwent single-shot turbo spin echo abdominal scans of the liver with coronal (TR 917 ms, TE 80ms, flip angle 90, TSE factor 64, acq matrix 300x262, FOV 450mm, slice thickness 5mm) and transverse slice geometry. Both scans were performed twice using either camera-based triggering or bellows-based triggering resulting in a total of 4 scans per subject. Image quality of the resulting coronal images was scored by a technical expert on a 6-point scale. Slice alignment quality was assessed based on sagittal reformatted images from these coronal scans. Transverse scans were used to assess general performance and were qualitatively reviewed to check presence of artifacts. Respiratory signal quality was compared by a technical expert on the same scale (5 = perfect, 3 = clinically still acceptable, < 3 artifacts / false triggers).Results
Camera and MRI system could be operated simultaneously without degradation of either system’s performance, i.e. neither video and physiology/respiratory signals nor MR image quality were compromised. The camera physiology sensor system performed reliably for all examinations and on average of all comparable sets, the breathing signal quality was superior compared to the bellows sensor (Camera: 4.4 +/- 0.7 vs. Bellows: 3.3 +/- 1.1 ) (Fig.3). The camera respiratory signal quality was never below 3 while for the bellows signal quality was below 3 in 18% of the scans. Respiratory triggered scans obtained with the camera as respiratory sensor showed on average superior image quality when compared to the same scans acquired with the belt (4.3 +/- 0.6 vs. 3.3 +/- 0.9) (Fig. 4,5). Image quality improvements could be observed in geometric slice alignment and motion-induced saturation artifacts due to partly wrong slice excitation. Camera-based respiratory sensor-triggered images were observed to be consistently in a comparatively more complete exhale state (Fig. 4, 5).
Acknowledgements
No acknowledgement found.References
[1] Bartula et al., Camera-based system for contactless monitoring of respiration, IEEE EMBC, 2013
[2] Maclaren et al., Prospective motion correction using coil-mounted cameras: Cross-calibration considerations, MRM, 2017
[3] Cheng et al., Optical Motion Monitoring for Abdominal and Lung Imaging, ISMRM, 2017
Figures