2519
Measuring Abdominal Wall Muscle Deformation using MR Tissue TaggingLawrence Dougherty1, Pilla J. James1, and Anil Chauhan1
1Radiology, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
The current state of hernia repair relies heavily on clinical evaluation of patients, which is ultimately a poor predictor of outcomes for patients going into surgery. There are currently no reliable data, standard imaging modalities, or guidelines available to predict successful fascial closure in hernia repair. A method using MR tissue tagging with synchronous displacement of the abdominal wall was developed. This will allow analysis of the mechanical properties of muscle for noninvasive, diagnostic tool for pre-operatively predicting successful fascial closure in hernia repair.
Introduction
Two million abdominal surgeries are performed annually in the United States, and ventral hernia (VH) is among the most common and serious complications1. The incidence of VH is approximately 13%, but as high as 70% in high-risk populations1-3. Failed repairs generate un-closable midline defects that require mesh bridging - native fascia cannot be closed and the mesh is ‘bridged’ across the fascia. Bridging is a relevant and clinically meaningful outcome, since repairs fail in 44 to 100% of cases and significant costs are incurred4. The current state of hernia repair relies heavily on clinical evaluation of patients, which is ultimately a poor predictor of outcomes for patients going into surgery. There are currently no reliable data, standard imaging modalities, or guidelines available to predict successful fascial closure in hernia repair. A method had been developed that allows non-invasive assessment of muscle compliance using a device to deform the abdominal muscle combined with MR tissue tagging.Methods
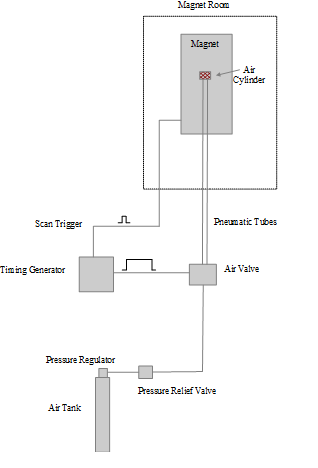
IRB approval was obtained prior to the start of this study and was HIPAA compliant. A custom device was built that deforms the abdominal wall muscle synchronous with the imaging cycle. Deformation was performed using an external device consisting of an MR compatible pneumatically actuated air cylinder (IPS, Irvive, CA) that was mounted to an RF coil. Pneumatic valves triggered by a timing board controlled the rates of extension and retraction of the air cylinder piston-rod (Figure 1). Maximum extension of the piston rod was 5 cm. The timing board also triggered the imaging sequence, which was a 2D SPGR gated multiphase acquisition with tissue tagging. Scan parameters were: TE=1.75ms, TR=3.9ms, FOV=320 x 210 mm, 4mm slice thickness, 6 mm tag spacing, using 5 views per cardiac segment. The sequence was gated to the air cylinder cycle time, which was 1800ms. The scan was performed in a breath-hold which was 27 seconds.Results
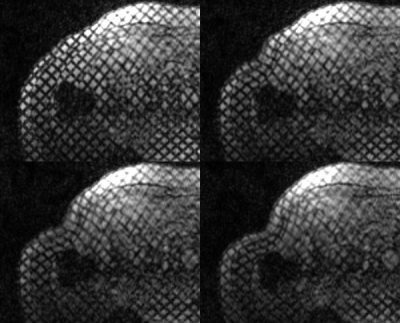
Five imaging studies were successfully performed on normal volunteers. The air cylinder was able to produce sufficient deformation of the abdominal wall muscle synchronous with the tissue tagged imaging sequence. Images from a volunteer study are shown in Figure 2. Muscle deformation is clearly seen in the final frames.Conclusion
MR tissue tagging with synchronous displacement of the abdominal wall was shown to provide measurements of muscle deformation. This will allow analysis of the mechanical properties of muscle for noninvasive pre-operative prediction of successful fascial closure in hernia repair.Acknowledgements
This work supported by an RSNA Research Seed Grant.References
- Poulose BK, Shelton J, Phillips S, et al. Epidemiology and cost of ventral hernia repair: Making the case for hernia research. Hernia. 2012;16:179-83.
- Mudge M, Hughes L. Incisional hernia: A 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70-1.
- Nho RLH, Mege D, Ouaïssi M, Sielezneff I, Sastre B. Incidence and prevention of ventral incisional hernia. Journal of visceral surgery. 2012;149:e3-e14.
- Bower C, Roth JS. Economics of abdominal wall reconstruction. Surg Clin North Am. 2013;93:1241-53.