2484
The workflow for the validation of USPIO-enhanced MRI for the detection of lymph node metastases in rectal cancerRutger C.H. Stijns1, Bart W.J. Philips1, Chella van der Post2, Iris D. Nagtegaal2, Carla Wauters3, Luc J.A. Strobbe4, Fatih Polat4, Johannes H.W. de Wilt5, Stefan H.G. Rietsch6,7, Sascha Brunheim6,7, Stephan Orzada6, Harald H. Quick6,7, Jurgen F. Fütterer1, and Tom W.J. Scheenen1,6
1Radiology and Nuclear medicine, Radboudumc, Nijmegen, Netherlands, 2Pathology, Radboudumc, Nijmegen, Netherlands, 3Pathology, Cansius Wilhelmina hospital, Nijmegen, Netherlands, 4Surgery, Cansius Wilhelmina hospital, Nijmegen, Netherlands, 5Surgery, Radboudumc, Nijmegen, Netherlands, 6Erwin L. Hahn Institute for MR Imaging, University of Duisburg-Essen, Essen, Germany, 7High Field and Hybrid MR Imaging, University Hospital Essen, Essen, Germany
Synopsis
For patients with rectal cancer, the presence of lymph node metastases is an important risk factor for determining prognosis and stratifying for treatment. Clinically, lymph node staging is very challenging, especially when lymph nodes are small (<5mm). By using ultrasmall superparamagnetic iron oxide (USPIO) particles combined with (ultra) high magnetic field imaging (combidex-enhanced MRI), the detection rate of these metastatic lymph nodes may improve significantly. In this abstract we present the workflow for validating combidex-enhanced MRI by performing a node to node comparison of in vivo combidex-enhanced MRI findings with histopathological examination.
Synopsis
For patients with rectal cancer, the presence of lymph node metastases is an important risk factor for determining prognosis and stratifying for treatment. Clinically, lymph node staging is very challenging, especially when lymph nodes are small (<5mm). By using ultrasmall superparamagnetic iron oxide (USPIO) particles combined with (ultra) high magnetic field imaging (combidex-enhanced MRI), the detection rate of these metastatic lymph nodes may improve significantly. In this abstract we present the workflow for validating combidex-enhanced MRI by performing a node to node comparison of in vivo combidex-enhanced MRI findings with histopathological examination.Introduction
The presence of lymph node metastases in rectal cancer is a key factor in determining an adequate treatment. Concluding on the lymph node status, however, is a major challenge.1 Ferumoxtran-10, an ultrasmall superparamagnetic iron oxide (USPIO) particle, has proven to be a valuable contrast agent for detecting lymph node metastases using MRI, also called combidex-enhanced MRI.2 Previous work showed that the diagnostic accuracy for the detection of small lymph node metastases (<5mm) dropped substantially.3 By using a 3 and 7 Tesla MRI scanner, it is possible to increase the spatial resolution of combidex-enhanced MRI, thereby increasing the sensitivity for the detection of small positive nodes.4 Histopathological validation of these nodes demands for a dedicated workflow from initial detection during in vivo MRI up to final histopathological examination. Here, we present the workflow and initial results in validating combidex-enhanced MRI for detecting small lymph node metastases in rectal cancer.Methods
In this observational study, patients with biopsy proven rectal cancer are included 1-2 weeks prior to surgical treatment. Patients are administered with 2.6 mg/kg body weight of ferumoxtran-10 mixed with 0.9% saline solution. 24-36 hours later an MRI examination is performed at 3T and at 7T (Magnetom Prisma and 7T, Siemens Healthineers, Erlangen, Germany). The MR protocol and parameters are displayed in Table 1.5 The detection of the lymph nodes is done on lipid-selective T1-weighted gradient echo MR images and the suspicion on metastatic manifestation is determined on T2*-weighted images6. Surgical treatment consists of a total mesorectal excision, in which the rectum including surrounding fatty tissue with lymph nodes is removed. After fixation in formalin, the surgical specimen is examined on a 7 Tesla preclinical MR system (ClinScan, Bruker® BioSpin, Ettlingen, Germany). These ex vivo MR images are used to annotate lymph nodes for an MR-guided pathological examination. The annotations enable a node-to-node comparison between in vivo MRI and pathology. The histopathological analysis is then used to validate the results of the 3T and 7T MRI scans. A complete overview of the workflow is given in Figure 1.Results
Three patients have been included in this ongoing study. Two patients underwent 3T MRI and 7T MRI and one patient underwent 3T MRI only. Two patients were scheduled for direct surgical treatment and one patient had received preoperative chemoradiotherapy. In these three patients 9 lymph nodes were considered malignant with a mean diameter of 4.1 mm (range 2 - 5 mm, example shown in Figure 2). The 7T ex vivo MRI scans revealed 146 lymph nodes with a mean diameter of 2.7 mm (range 0.8 – 5.2 mm). Histopathological examination harvested 48 lymph nodes from the surgical specimens, including the 9 lymph nodes suspicious for metastases based on combidex-enhanced MRI. 8 out of 9 suspicious nodes could be matched to histology as visualized in Figure 3.Discussion
The preliminary data of the ongoing study shows that it is feasible to visualize potentially malignant lymph nodes in rectal cancer patients by using combidex-enhanced MRI. Both 3T and 7T MRI showed that the contrast agent can migrate to lymph nodes after an intravenous infusion. Preoperative chemoradiotherapy may impede the transport of the nano-particles towards the locoregional lymph nodes, which has to be explored in future patients. By using our current workflow, we are able to identify the potentially metastatic lymph nodes at initial in vivo MRI and keep track of them all the way to the histological slide at pathology. The additional step of the 7T ex vivo MRI scan allows the node-to-node correlation between the in vivo MRI images and histology. This extra step in the workflow is of great value in determining the accuracy of combidex-enhanced MRI on a lymph node basis. The lymph nodes with a high suspicion of malignancy can be identified ex vivo and pointed out during work-up for histological examination, thereby enabling the pathologist to make a final statement on the lymphatic spread of the cancer and on the predictive value of combidex-enhanced MRI for rectal cancer staging.Acknowledgements
No acknowledgement found.References
1. Beets-Tan RGH, Lambregts DMJ, Maas M, et al. Magnetic resonance imaging for clinical management of rectal cancer: Updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. European radiology 2017. 2. Fortuin AS, Bruggemann R, van der Linden J, et al. Ultra-small superparamagnetic iron oxides for metastatic lymph node detection: back on the block. Wiley interdisciplinary reviews Nanomedicine and nanobiotechnology 2017. 3. Harisinghani MG, Barentsz J, Hahn PF, et al. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. The New England journal of medicine 2003;348:2491-9. 4. Heesakkers RA, Futterer JJ, Hovels AM, et al. Prostate cancer evaluated with ferumoxtran-10-enhanced T2*-weighted MR Imaging at 1.5 and 3.0 T: early experience. Radiology 2006;239:481-7. 5. Orzada S, Maderwald S, Poser BA, Bitz AK, Quick HH, Ladd ME. RF excitation using time interleaved acquisition of modes (TIAMO) to address B1 inhomogeneity in high-field MRI. Magnetic resonance in medicine 2010;64:327-33. 6. Philips BWJ, Fortuin AS, Orzada S, Scheenen TWJ, Maas MC. High resolution MR imaging of pelvic lymph nodes at 7 Tesla. Magnetic resonance in medicine 2017;78:1020-8.Figures
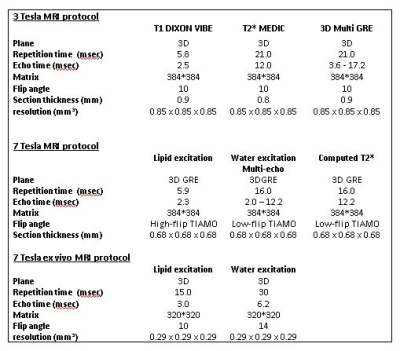
Table 1 - Imaging parameters of the 3
and 7 Tesla MR protocols.
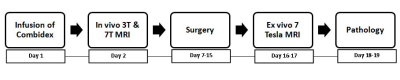
Figure 1 - Workflow of the study.
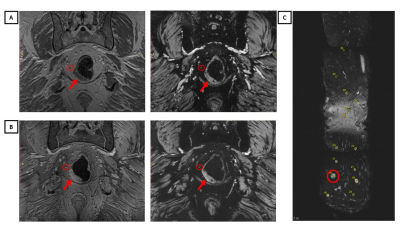
Figure
2 –3 Tesla (A) and 7 Tesla MRI (B) scan in the
coronal plane of a patient with rectal cancer after the administration of
Combidex. In the left lipid image (A+B) the red
circle points out a lymph node. The right computed TE12.2 ms GRE image (A+B) from
the multi-GRE acquisition displays the same node as a hyperintense suspicious
lymph node (red circle). The red arrow indicates the primary tumour. The ex
vivo MRI (C) enabled matching of the in vivo MRI images with histology, which
revealed the suspicious node to be metastatic with extranodal tumor growth.
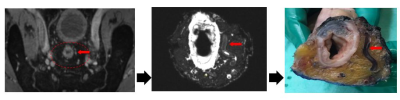
Figure 3 – Example of the workflow
from in vivo MRI to histopathology. Left displays the in vivo MRI image, in the
middle the ex vivo MRI images and on the right the surgical specimen. The red
arrow indicates a blood vessel which that was used as a landmark during
node-to-node matching.