2463
Machine learning of DCE MRI intensity histogram radiomic features for pulmonary lesion classification1Radiology, Tongji Medical college affiliated to Huazhong University of Science and Technology, Wuhan, China, 2Radiation Oncology, University of Washington, Seattle, WA, United States, 3Radiology, University of Washington, Seattle, WA, United States
Synopsis
To classify malignant/benign lesions can be challenging and non-invasive means to further improve the diagnostic accuracy would have major impact on management in patients with pulmonary lesions. 62 patients with histologically confirmed pulmonary lesions were retrospectively reviewed. Intensity voxel histogram (IH) features were extracted from DCE-MRI. The efficacy of IH features to classify pulmonary lesions were assessed by correlation with pathology. Under cross-validation, a support vector machine algorithm achieved a diagnostic accuracy, sensitivity and specificity of 95%, 99 and 86%. Our results demonstrate that machine learning of DCE-MRI IH features has potential for accurately classifying pulmonary lesions for clinical translation.
Introduction
Lesion diagnosis on DCE MRI has been primarily limited to kinetic and morphologic variables. Recently, image intensity histogram analysis based on tumor voxel distributions was introduced as a possible diagnostic tool for tumor discrimination, tumor grading or treatment response evaluation by reflecting the underlying lesion biologic heterogeneity.1,2,3 In this work, we evaluate whether machine learning of DCE MRI intensity histogram radiomic features can further improve the differentiation between malignant and benign pulmonary lesions in a novel manner compared to conventional kinetic and morphologic variables.Methods
With IRB approval and informed consent waived, 62 patients with pulmonary lesions (benign/malignant = 18/44) who underwent DCE MRI scans obtained with 1.5 T units or 3T units and subsequently had histopathologic confirmation were included in our study. Routine MR scans prior to DCE-MRI consisted of T1-and T2-weighted images obtained in the transverse plane in each patient. DCE MR scans consisted of a transverse orientation dynamic sequence using liver acquisition of volume acceleration (LAVA) with 30 sec temporal sampling, repeated for 18 frames, yielding a total acquisition time of 540 sec. Contours defining the whole 3D lesion region for each patient were manually delineated slice-by-slice on the axial pre-contrast and contrast-T1 images by a chest radiologist in MIM 6.6TM (MIM Software Inc., Cleveland, OH). Time-intensity curves were generated and the peak enhancement phase was manually selected. The peak enhancement phase images were subsequently fused with the pre-enhancement images to produce the enhancement ratio images. Nine intensity histogram features, including volume, integral, maximum, minimum, mean, median, kurtosis, skewness and the coefficient of variation (CoV) were extracted from the enhancement ratio images via MIM.1 Univariate receiver operating characteristic models, as well as multivariate support vector machine (SVM) models with radial basis function (RBF) kernels, were generated to predict the lesions’ pathological diagnosis (benign vs. malignant). Diagnostic performance was evaluated using leave-1-out cross-validation and averaged over 5 independent realizations.
Results
CoV was significantly higher in benign pulmonary lesions with AUC = 0.78 (P=0.001) (Table 1). When combining all histogram features, the SVM-RBF model achieved a 5-run average diagnostic accuracy of 94.8%, with sensitivity of 98.6%, specificity of 85.6%, positive predictive value of 94.4% and negative predictive value of 96.3% (Table 2). CoV ranked highest in importance for the SVM-RBF model, followed by volume, median, integral, mean, maximum, kurtosis, skewness and minimum (Table 3).Discussion
In our study, we included a variety of benign nodule types (active infectious as well as the other benign lesions), which made the lesion classification more difficult using a single metric. CoV was the only variable which could successfully differentiate the malignant and benign groups. The examples (Figures 1 and 2) show a pair of benign and malignant cases with similar visual morphology and enhancement patterns but different intensity histogram features. In the multivariate analysis using leave-one-out cross validation with SVM-RBF machine learning algorithm, we combined intensity histogram features to further improve classification. We found that the SVM-RBF model can reach high diagnostic accuracy of 95%, with sensitivity of 99% and specificity of 86%. Our internally validated prediction model also showed reasonable consistency and stability over multiple independent realizations. This compares well with prior DCE-MRI studies on lesion classification that reported sensitivity, specificity and accuracy of 76-100%, 70-100%, and 80-95%, respectively,4 including use of a multiparametric approach.5Conclusion:
Our suggests the potential power of machine learning with DCE MRI intensity histogram radiomic features to further improve the classification of benign versus malignant pulmonary lesions. The coefficient of variation of perfusion in the peak enhancement phase can differentiate between the two groups more accurately than the conventional metrics of mean peak enhancement, median peak enhancement or lesion volume. Machine learning of intensity histogram features can account for variability in perfusion patterns of benign lesions and aid in diagnostic performance.Acknowledgements
No acknowledgement found.References
1. Bowen SR, Yuh WTC, Hippe DS, et al. Tumor radiomic heterogeneity: Multiparametric functional imaging to characterize variability and predict response following cervical cancer radiation therapy. J Magn Reson Imaging 2017; 1805:105.
2. Pixel Analysis of MR Perfusion Imaging in Predicting Radiation Therapy Outcome in Cervical Cancer. 2000:1–7.
3. Young R, Babb J, Law M, Pollack E, Johnson G: Comparison of region-of-interest analysis with three different histogram analysis methods in the determination of perfusion metrics in patients with brain gliomas. J Magn Reson Imaging 2007; 26:1053–1063.
4. Khalil A, Majlath M, Gounant V, et al. Contribution of magnetic resonance imaging in lung cancer imaging. Diagnostic and Interventional Imaging 2016; 97:991–1002.
5. MD JB, MD AL, PhD JS-G, et al. Functional MR Imaging in Chest Malignancies. Magnetic Resonance Imaging Clinics of NA 2016; 24:135–155.
Figures
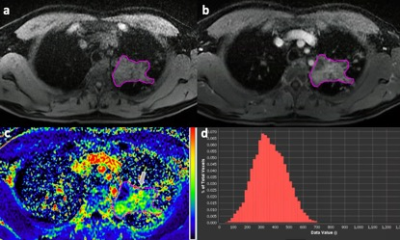
Figure 1. A 51 years old male patient with a 5 cm mass in left upper lobe and confirmed to be tuberculosis
a. Pre-contrast T1-WI showing an irregular mass with homogeneous low to medium signal intensity
b. Post-contrast T1-WI at peak enhancement phase showed the mass with increased heterogeneous enhancement
c. DCE enhancement ratio image at peak enhancement phase showing the mass with heterogeneous perfusion
d. Voxel histogram of the ratio image showed a dispersed and broader distribution with higher perfusion
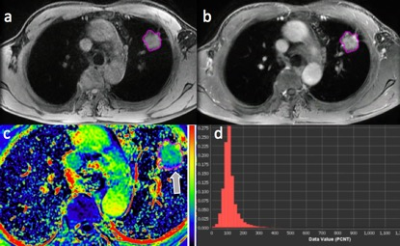
Figure 2. A 56 years old male patient with a 2.8 cm nodule in left upper lobe and confirmed to be adenocarcinoma
a. Pre-contrast T1-WI showing a lobular nodule with homogeneous intermediate signal intensity
b. Post-contrast T1-WI at peak enhancement phase showing the lobular nodule with heterogeneous enhancement
c. DCE enhancement ratio image at peak enhancement phase showed the nodule with intra-tumoral heterogeneous perfusion
d. Voxel histogram of the ratio image showing a more compact and peaked distribution of malignant lesion compared to the benign lesion (Fig 1)
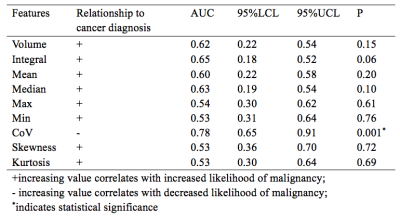
Table 1. Univariate receiver operator characteristic analyses of 9 features
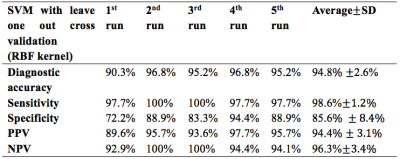
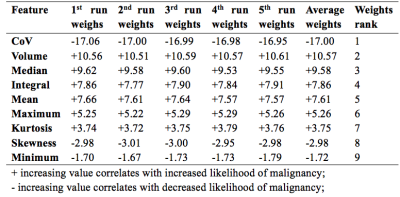
Table 3. Weights for each run and the rank of the weights for 9 features in classification