2447
Fetal non-contrast MR angiography in second and early third trimesterUday Krishnamurthy1, Swati Mody1, Brijesh Yadav1, Pavan Kumar Jella1, Edgar Edgar Hernandez-Andrade2,3, Anabela Trifan1, Ewart Haacke1, Roberto Romero3, and Jaladhar Neelavalli1
1Radiology, Wayne State University, Detroit, MI, United States, 2Obstetrics and Gynecology, Wayne State University, Detroit, MI, United States, 3Perinatology Research Branch, NICHD/NIH/DHHS, Detroit, MI, United States
Synopsis
To evaluate the robustness and utility of non-contrast MRA as a means to visualize fetal vasculature, particularly in fetuses younger than 30 weeks gestation.
Introduction
Recent studies have shown the feasibility of using non-contrast time of flight (TOF) [1] MRA in older and near term fetuses. However, the diagnostic quality and the conspicuity of the fetal vessels have not been evaluated. Furthermore, due to concerns of motion, it is challenging to consistently obtain diagnostic image quality in younger gestation fetuses. Lately, non-Cartesian sequences are being developed to address the concerns of motion [2]. However, they too fail in providing diagnostic image quality under cases of extreme motion, which is more common in second and early third trimester fetuses. Hence, in this work our goal was to systematically assess the quality of non-contrast MRA technique in fetuses younger than 30 weeks. Specifically, we evaluated the conspicuity of the major fetal vessels and the diagnostic quality of the maximum-intensity projections (MIPS) and the raw slice-by-slice data.Methods
A total of 16 healthy fetus younger than 30 weeks gestation were scanned on a Siemens Verio (3.0T field strength) using a 6 channel body flex coil and the spine coil. The fetal heart and the major branches were consistently included in the field-of-view. A fully flow compensated 2D gradient echo sequence with Cartesian sampling and with the parameters reported previously [1]. An additional radial MRA scan was obtained in 5 fetuses with the parameters reported previously [2]. The radial scans had a higher in-plane resolution of 0.5mm. All data was reconstructed to create 3D vascular projections using OSIRIX [3]. The raw data and the maximum intensity projections (MIPS) were evaluated for diagnostic quality on a 5 point Likert scale (where 0- Non-diagnostic; 1- Poor ; 2- Fair; 3- Good; 4-Excellent image quality) and conspicuity of major vessels/structure (Aorta, Inferior venecava, umbilical arteries, umbilical veins, ductus venous, major neck vessels, hepatic vessels) on a similar 3 point scale (0- Not-visible; 1-Blurred; 2- Distinct) by a trained pediatric radiologist (SM) with more than 12 years of experience in reading fetal MRI. In case of both Cartesian and radial data being available the better of the two was chosen to represent the case.Results
Representative MIPS and raw images indicating the image quality are demonstrated in Figure 1. Seventy five percent (12/16) of the MIPS were scored as diagnostic (scores of 2 and above), and 62% of the raw data was scored as diagnostic. A complete scoring scheme is highlighted in Figure 2. When looking at individual structures, the edge definition and ability to distinguish them, in almost all the cases a maximum of them were distinct (Figure 3). The visibility of the ductus venous was the poorest and could not be identified in roughly 19% of the cases, followed by the septum of heart and the major vessels of neck both were not identifiable in 12.5% of the scans.Discussions and Conclusions
The 2D TOF technique provides a good suppression of fetal background and high sensitivity to the inflow effects. The above results indicate that it is possible to get diagnostic images in 75% of the cases in younger second and early third trimesters, usually higher than those reported with other sequences used for fetal imaging [4]. The resolution of 0.7 mm was sufficient to distinctly identify and detect most fetal vessels in the thorax & abdomen. Motion remains an issue when creating the MIPS however the individual slices were themselves not severely affected, as is evident by the cases that received scores of 4 & 5 for raw data. Severe motion, however, affected the quality of the individual slices and thereby the MIPS as well. In conclusion, MRA even in younger gestational ages provides diagnostic quality images and may be translated into clinical settings to study vascular malformations. Future works that can include slice-to-volume registration [5] would alleviate the slice motion artifacts and provide high quality 3D visualizations of the vascular tree.Acknowledgements
No acknowledgement found.References
[1] Neelavalli, J, et al. European radiology 26.12 (2016): 4570-4576. [2] Krishnamurthy, U, et al. ISMRM 2017 [3] Rosset, Antoine, et al. Journal of digital imaging 17.3 (2004): 205-216. [4] Cortes, et al. Fetal diagnosis and therapy 41.2 (2017): 127-135. [5] Lloyd, David, et al. Journal of Cardiovascular Magnetic Resonance 18.1 (2016): P180.Figures
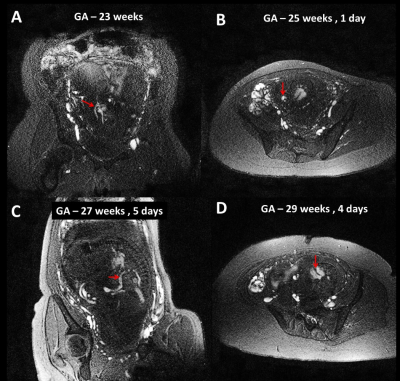
Figure 1: Raw single slice views (2 mm thickness) of the major fetal vessels shown across the spectrum of younger gestational ages. Gestational Ages A – 23 weeks (Arch of aorta, Inferior veneceva, heart and hepatic vein); B – 25 weeks 1 day (Umbilical artery and vein, septum of heart, aorta & major branches); C – 27 weeks and 5 days (Ductus venous, Umbilical artery, heart and major neck vessels); D – 29 weeks 4 days (Septum of heart, umbilical artery and vein). Note the size of the fetal vessels and the suppression of fetal and background structures.
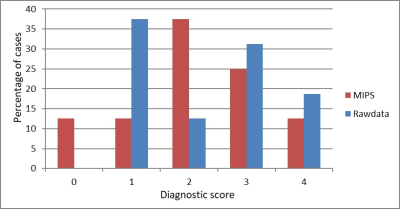
Figure 2: Diagnostic Quality score of MIPS (red) and Rawdata (Blue). The scores correspond to 0- Non-diagnostic; 1- Poor Quality; 2- Fair; 3- Good; 4-Excellent
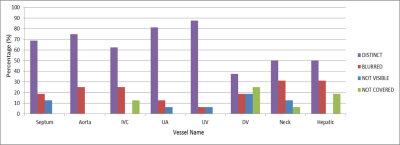
Figure 3: Scores of conspicuity of major fetal vessels. The scores correspond to 0- Not-visible (blue); 1-Blurred (red); 2- Distinct (purple); 3 – Not included in the anatomical field-of-view (green). IVC – Inferior venecava. UA – umbilical artery; UV – umbilical vein; DV – ductus venosus.