2446
Design of a 36-channel receive coil array for fetal MRI at 3T1Lauterbur Imaging Research Center, Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, 2Shenzhen Key Laboratory for MRI, Shenzhen, China, 3School of Basic Science, Guangzhou Medical University, Guangzhou, China, 4High-Field Magnetic Resonance Brain Imaging Key Laboratory of Sichuan Province, School of Life Science and Technology, University of Electronic Science and Technology of China, Chengdu, China, 5Shenzhen People's Hospital, Shenzhen, China, 6Department of Radiology and Biomedical Imaging, University of California San Francisco, San Francisco, CA, United States, 7UCSF/UC Berkeley Joint Graduate Group in Bioengineering, San Francisco, CA, United States
Synopsis
Due to lack of dedicated fetal imaging coils, the standard commercial abdominal coil is often used for fetal imaging, of which the performance is limited by its insufficient coverage and element number. In this work, a dedicated 36-channel coil array for fetal imaging was designed, capable of covering a range of pregnancy from 20 to 37+ weeks. Compared to a commercial abdominal coil array, the proposed 36-channel fetal coil provides improved performance in SNR, parallel imaging capability, and image quality.
Introduction
MRI has been recognized as an important complementary tool to ultrasound for the diagnosis of fetal malformations, due to its superior soft tissue contrast and capability of large FOV scan to show entire body of fetus1. However, the abdomen of pregnant women is larger than that of normal people, the commercially available abdomen coil array is not optimal for fetal MRI in term of coverage and flexibility. Previous studies with specially-made coils have demonstrated highly accelerated fetal imaging at 3T, which shows a potential application of MRI in fetal imaging2, 3. In this work, we designed and built a 36-channel received coil for fetal MRI at 3T with a large coverage and flexibility, of which the imaging performance was evaluated in comparison with a commercially available 18-channel abdomen coil array which is often used for fetal imaging.
Methods
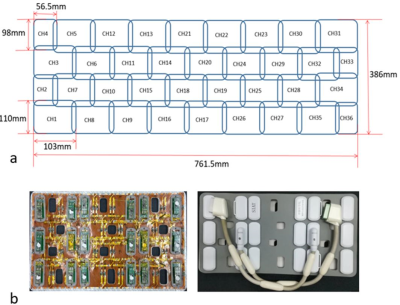
The layout of the 36-channel coil and the prototype coil array are shown in Figure 1, in which the sizes of channel 2, 4, 33 and 36 were 98 mm x 56.5 mm and the others were 110 mm x 103 mm. Here, the decoupling methods of overlapping adjacent coil elements and employing low input-impedance preamplifiers were applied. Each element was tuned to 123.2 MHz and impedance-matched to minimize the noise of the preamp. To maintain the flexibility and gain the durability and safety, the coil array was covered by the polyethylene material. Bench testing was carried out with the coil element tuning, active detuning, decoupling with nearest-neighbor element by using a custom-made test power supply and a vector network analyzer. Phantom experiments of the 36-channel coil were firstly implemented on a SIEMENS Skyra 3 T system in comparison with a commercially available 18-channel abdomen coil array. In all experiments, a 12-channel coil from the 32-channel spine array was combined with both coils. Phantom images were acquired with a 2D GRE sequence (TR/TE=300 ms/10 ms, flip angle=60o, FOV= 400 mm, slice thickness=5 mm, Matrix size=256 x 256), of which results can be applied to compute covariance weighted SNR4 and SENSE g-factor maps5. Generally, the mean values of the combined SNR maps and the inverse g-factor maps were calculated to assess the coil array performance in several ROIs that the fetal brain and heart may appear for its motility. For fetal images, a 2D HASTE sequence was applied to obtain fetal brain images with parameters: TR/TE=1400 ms/92 ms, FOV=380 mm, slice thickness=3.5 mm, slices=20, flip angle=160o, matrix size=320 x 288, Bandwidth=710 Hz/Px, accelerate factor=2, phase partial Fourier=4/8. Notably, a high dielectric pad was placed beneath the pregnant woman during all the fetal imaging.Results
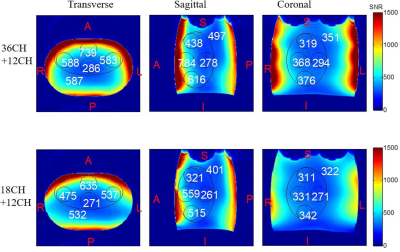
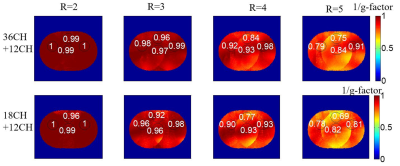
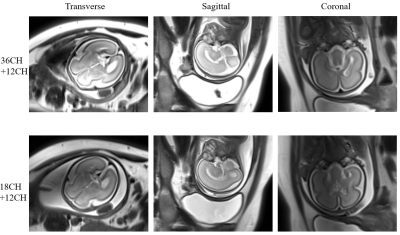
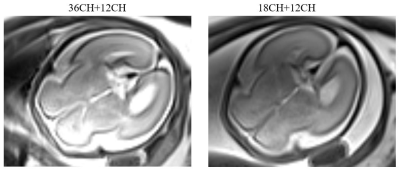
The average S-parameter was approximately -15 dB and the unloaded-to-loaded quality factor (Qunload to Qload) was 100/20, which indicated that the coils were well coupled to the imaging samples. The SNR distributions from phantom images in the transverse, sagittal and coronal planes were showed in Figure 2, from which it can be known that the 36-channel fetal coil achieved an average of 10% in the largest ROIs (at least 6% in the center region and up to 40% in the edge region) SNR improvement as compared to the 18-channel abdominal coil. Figure 3 depicted the inverse g-factor maps in the transverse plane with acceleration factors from 2 to 5 in the Right/Left (R/L) direction. Obviously, the proposed 36-channel coil showed a better parallel imaging capability than that of the 18-channel coil, particularly at the acceleration factors of 4 and 5. The fetal images obtained from a 24 weeks pregnant woman at 3 T were illustrated in Figure 4. In the fetal brain area shown in Figure 5, the proposed 36-channel fetal coil had higher signals than that acquired by using the commercial abdominal coil.Discussion
The SNR improvement in the center regions of the full phase encoding images was not very significant for the 36-channel fetal coil over that of the commercial abdominal coil, which is most likely due to a smaller size of each resonant element of the coil array. Nevertheless, the 36-channel fetal coil showed a better performance in parallel imaging than the 18-channel fetal coil because of the higher channel number. Further work is needed to be done in the SNR improvement in the center regions.Conclusion
A 36-channel array coil dedicated for fetal imaging was designed, constructed and evaluated by imaging experiments in phantoms and pregnant women. Compared to a commonly-used 18-channel abdominal coil for fetal imaging, the 36-channel coil achieves better performance in MR SNR, acceleration capacity and quality of fetal images.Acknowledgements
This work was supported in part by NSFC under Grant No. 61571433, 81527901, 81527901, 81327801, 81571669 and 81627901, Guangdong Province grants 2014A030313691, 2015B020214006 and 2014B030301013. Youth Innovation Promotion Association of CAS No. 2017415, city grants KQJSCX20160301143250, KQCX2015033117354154 and JCYJ20170413161314734 and a Pengcheng Scholar Award.References
1. Weisstanner C, Kasprian G, Gruber G M, et al. MRI of the Fetal Brain [J]. Clinical neuroradiology, 2015, 25(2): 189-196.
2. Ye Li, et al. Parallel MRI performance evaluation of a novel 32 channel fetal array at 1.5T, 20th ISMRM, 2012, 0568.
3. Mark Spatz, et al. A 64 Channel 3T Array Coil for Highly Accelerated Fetal Imaging at 22 Weeks of Pregnancy, 25th ISMRM, 2017, 1220.
4. Keil B, Wald L L. Massively parallel MRI detector arrays [J]. Journal of magnetic resonance, 2013, 229: 75-89.
5. Pruessmann K P, Weiger M, Scheidegger M B, et al. SENSE: sensitivity encoding for fast MRI [J]. Magnetic resonance in medicine, 1999, 42(5): 952-962.
Figures