2438
129Xe signal dynamics and chemical shift in the cardio-pulmonary circuit using cardiac-gated hyperpolarized 129Xe NMR1University of Sheffield, Sheffield, United Kingdom
Synopsis
The sensitivity of the 129Xe chemical shift to red blood cell oxygenation makes hyperpolarized 129Xe MR spectroscopy a promising technique for measurement of blood oxygenation in vivo. In addition, dissolved phase 129Xe MRS is of interest as a biomarker of gas exchange and interstitial lung disease. Both the signal dynamics and chemical shift of 129Xe have been shown to be modulated by the cardiac cycle, potentially adding confounding effects to interpretation of the 129Xe MRS chemical shift. In this study, we demonstrate that cardiac-gating in 129Xe MRS reduces the variability in the measured dissolved 129Xe signal and chemical shift in the cardio-pulmonary circuit.
Introduction
MR imaging and spectroscopy of 129Xe dissolved in pulmonary red blood cells (RBCs) and parenchymal tissue/plasma (TP) is of interest for investigating gas exchange limitation in interstitial lung diseases.1,2 Key to the success of dissolved-phase 129Xe spectroscopy and imaging is the ability to reliably measure the signal amplitude and chemical shift of 129Xe in red blood cells (RBCs) within an MR acquisition. Both the signal amplitude and chemical shift of 129Xe dissolved in RBCs have been shown to be modulated by cardiac pulsation.3 This has implications for accurate measurement of RBC oxygenation from the 129Xe chemical shift, Dixon-based dissolved 129Xe imaging, which assumes a fixed chemical shift difference between the target RBC and TP compartments, and for 129Xe MRS techniques which depend on robust quantification of the RBC and TP signals as biomarkers for gas exchange efficiency.4 In this study, we demonstrate the use of cardiac-gated pulmonary spectroscopy to mitigate previously observed modulations in the 129Xe-RBC signal and chemical shift.Methods
Hyperpolarized 129Xe pulmonary MRS was performed on a healthy male volunteer on a clinical 3 T (Philips, Achieva) scanner with a quadrature flex T-R coil (CMRS). All scans were performed at breath-hold apnoea after inhalation (from functional residual capacity) of 500 mL of hyperpolarized 129Xe balanced with 500 mL of medical-grade N2. Two sequences were implemented with the following parameters: hard pulses centered on the 129Xe-RBC resonance, flip angle = 90°, spectral points = 256, bandwidth = 3 kHz. The first sequence was performed with a fixed RF pulse delay of TR = 500 ms. In the other sequence, RF pulses were ECG triggered at end ventricular diastole. The 129Xe signal in RBCs and TP was determined by performing zeroth-order phasing on the associated resonances followed by numerical integration between the y-axis zero crossings on either side of the resonant peaks as it was not possible to obtain a good fit due to the non-Lorentzian behavior of the RBC resonance. The 129Xe-RBC chemical shift was determined using 0 ppm as a reference for 129Xe-TP.Results and Discussion
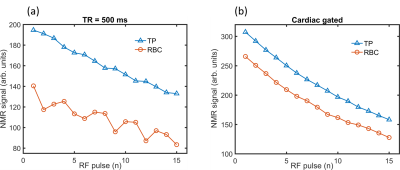
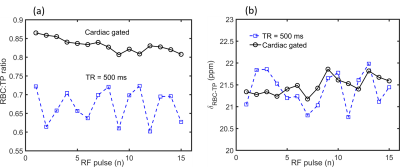
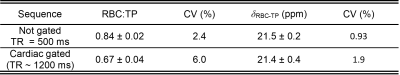
The 129Xe-RBC and 129Xe-TP signals were observed to decay during both MR acquisitions with a time constant characteristic of 129Xe-gas in the alveolar reservoir (Fig. 1 (a) to (d)); after each saturation pulse, the dissolved compartments are replenished with 129Xe gas from the alveoli with polarization that is undergoing T1 decay (T1 = 18.8 s). The mean RBC:TP peak ratios and 129Xe-RBC chemical shifts were calculated to be 0.84 ± 0.02 and 0.67 ± 0.04 and 21.5 ± 0.2 ppm and 21.4 ± 0.04 ppm using cardiac-gated and standard pulse sequences, respectively – see Figure 1 and Table 1. The coefficient of variation (CV), defined as the standard deviation divided by the mean value, is a factor of 2.5 higher for the RBC:TP ratio and a factor of 2 higher for the 129Xe-RBC shift with the non-gated sequence when compared to the cardiac-gated sequence. The lower CV values observed using cardiac gating can be attributed to sampling the 129Xe-RBC signal at a fixed period within the cardiac cycle where there should be a fixed and repeatable influx of oxygen desaturated blood entering the alveolar capillary bed from the right ventricle when compared to the non-gated pulse sequence where the blood flux and RBC oxygenation will be less consistent due to incoherent signal sampling with respect to the cardiac cycle. The larger RBC:TP ratio calculated with the cardiac gated sequence is likely due to more blood volume being sampled downstream of the alveolar-capillary gas exchange surface, as the patient’s heart rate was ~50 beats/minute giving an effective TR = 1200 ms when compared to TR = 500 ms with the non-gated sequence; it has being shown previously5 that the RBC:TP ratio increases with TR, plateauing at TR~3000 ms.Conclusion
129Xe cardiac gated pulmonary MR sequences provide more reliable measurements of the RBC:TP ratio and the 129Xe-RBC shift when compared to sequences that acquire the 129Xe signal at random phases of the cardiac cycle. This has implications for Dixon-based imaging dissolved 129Xe MRI and 129Xe MRS techniques where accurate values of 129Xe-RBC shift and RBC:TP ratio are needed.Acknowledgements
This work was supported by NIHR grant NIHR-RP-R3-12-027 and MRC grant MR/M008894/1. The views expressed in this work are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of HealthReferences
1. Wang Z, et al. Quantitative analysis of hyperpolarized 129Xe Gas Transfer MRI. Medical Physics. 2017; 44(6):2415-2428.
2. Kaushik SS, et al. Measuring diffusion limitation with a perfusion-limited gas—Hyperpolarized 129Xe gas-transfer spectroscopy in patients with idiopathic pulmonary fibrosis. Journal of Applied Physiology. 2014;117(6):577-85.
3. Norquay G, et al. 129Xe chemical shift in human blood and pulmonary blood oxygenation measurement in humans using hyperpolarized 129Xe NMR. Magnetic Resonance in Medicine. 2017; 77(4):1399-1408.
4. Stewart NJ, et al. Reproducibility and Methodological Considerations for Dissolved-Phase 129Xe Spectroscopy in Patients with Idiopathic Pulmonary Fibrosis. Proc. ISMRM, Honolulu, US. 2017; p21485.
5. Norquay G, et al. Evaluation of 129Xe-RBC signal dynamics and chemical shift in the cardiopulmonary circuit using hyperpolarized 129Xe. Proc. ISMRM, Honolulu, US. 2017; p3327.
Figures